|
||||||||||||
Malignant
Disease: Staging
of Gynecologic Application
of Vaginal Application
of Uterine Afterloading Applicators Abdominal
Injection of Chromic Phosphate Radical
Vulvectomy Reconstruction
of the Transverse
Rectus Colonic
"J" Pouch Rectal Ileocolic Continent Urostomy (Miami Pouch) Construction
of Neoanus Skin-Stretching
System Versus Skin Grafting Gastric
Pelvic Flap for Control
of Hemorrhage in Gynecologic Surgery Repair
of the Punctured Ligation
of a Lacerated Hemorrhage
Control in Presacral
Space What
Not to Do in Case of Pelvic Hemorrhage |
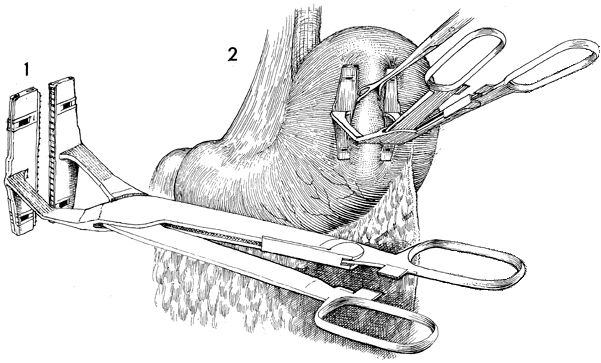
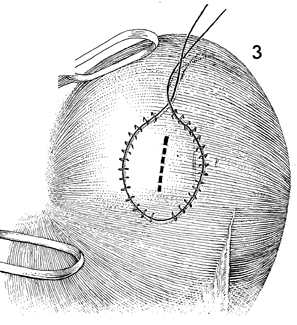
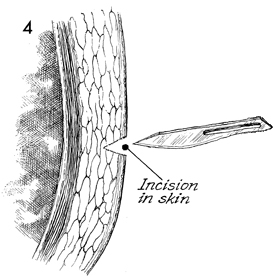
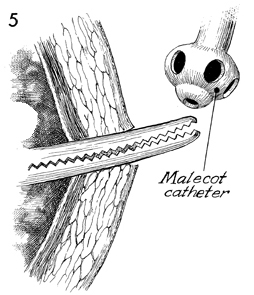
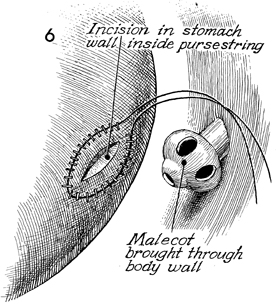
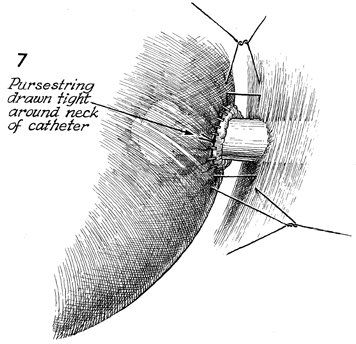
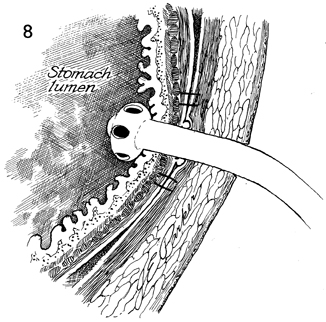
Tube Gastrostomy A tube gastrostomy can be used following extensive gastrointestinal surgery to decompress the intestines and, when indicated, to supply enteral nutrition. Physiologic Changes. The gastrostomy tube decompresses the stomach and, while the adynamic process is in place, prevents air from passing into the small bowel. Hydrochloric acid is removed from the stomach. The volume of secretions removed from the stomach should be replaced intravenously with sodium chloride. The alternative to tube gastrostomy is a nasogastric tube. This is a space-occupying mass in the mediastinum. The tube gastrostomy eliminates the need for a nasogastric tube, thereby reducing dead space and improving respiratory function. Points of Caution. Care must be taken to see that the gastrostomy tube is within the lumen of the stomach and has not been pulled back into the peritoneal cavity. This is accomplished by suturing the parietal peritoneum to the visceral peritoneum surrounding the gastrostomy and placing skin sutures to the gastrostomy tube. Technique
|
|||||||||||
Copyright - all rights reserved / Clifford R. Wheeless,
Jr., M.D. and Marcella L. Roenneburg, M.D.
All contents of this web site are copywrite protected.