Malignant
Disease:
Special Procedures
Staging
of Gynecologic
Oncology Patients With
Exploratory Laparotomy
Subclavian Port-A-Cath
Peritoneal Port-A-Cath
Application
of Vaginal
Cylinders for Intracavitary
Radiation Therapy
Application
of Uterine Afterloading Applicators
for Intracavitary Radiation Therapy
Pelvic High-Dose
Afterloader
Abdominal
Injection of Chromic Phosphate
( ) )
Supracolic
Total Omentectomy
Omental Pedicle "J"
Flap
Tube Gastrostomy
Total Vaginectomy
Radical
Vulvectomy
With Bilateral Inguinal
Lymph Node Dissection
Reconstruction
of the
Vulva With Gracilis Myocutaneous Flaps
Transverse
Rectus
Abdominis Myocutaneous
Flap and Vertical Rectus
Abdominis Myocutaneous
Flap
Radical
Wertheim
Hysterectomy With
Bilateral Pelvic Lymph
Node Dissection and With Extension of the Vagina
Anterior Exenteration
Posterior Exenteration
Total Pelvic
Exenteration
Colonic
"J" Pouch Rectal
Reservoir
Kock Pouch
Continent Urostomy
Omental "J" Flap
Neovagina
Ileocolic
Continent Urostomy (Miami Pouch)
Construction
of Neoanus
Gracilis Dynamic Anal
Myoplasty
Skin-Stretching
System Versus Skin Grafting
Gastric
Pelvic Flap for
Augmentation of Continent Urostomy or Neovagina
Control
of Hemorrhage in Gynecologic Surgery
Repair
of the Punctured
Vena Cava
Ligation
of a Lacerated
Internal Iliac Vein and
Suturing of a Lacerated Common Iliac Artery
Hemorrhage
Control in
Sacrospinous Ligament
Suspension of the Vagina
Presacral
Space
Hemorrhage Control
What
Not to Do in Case of Pelvic Hemorrhage
Packing
for Hemorrhage
Control
Control
of Hemorrhage
Associated With Abdominal Pregnancy |
Control of Hemorrhage Associated
With Abdominal Pregnancy
Control of hemorrhage associated with abdominal pregnancy is an important
technique in obstetrical care. Every labor or delivery room should
have a protocol as to the management of abdominal pregnancy. There
are several available protocols, but none is perfect, and all have
sequelae and long-term complications.
Technique
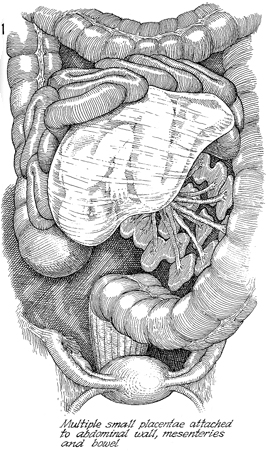
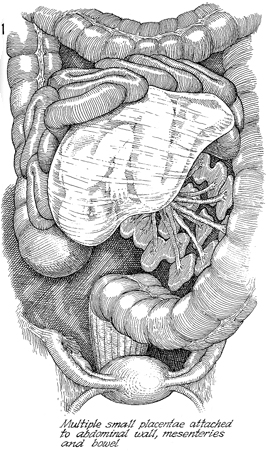
In this patient, the fetus shows multiple
placental attachments to the mesentery of the descending colon.
In this patient also, the placentae are attached in one particular
area. Placentae can be attached all over the abdomen, however,
from the liver to the pelvis. Each of these placentae has its
own blood supply. |
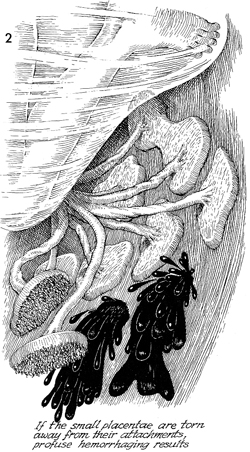
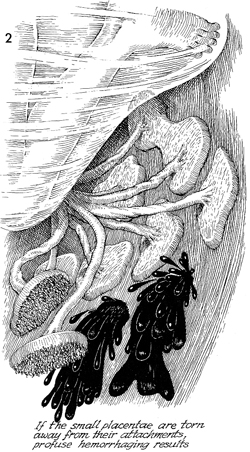
Several of the placentae have been dislodged
and torn away from the attachments. Profuse hemorrhage results.
Individual clamping or ligating of these hemorrhaging sites is
frequently impossible. The most efficacious management of this
problem is to clamp the main umbilical cord immediately adjacent
to the fetus, remove the fetus, and pack off the bleeding sites
with large abdominal packs, sterile sheets, or whatever available. |
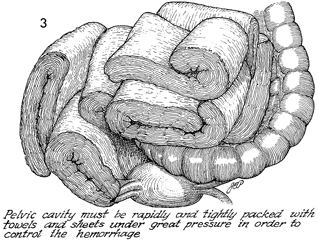
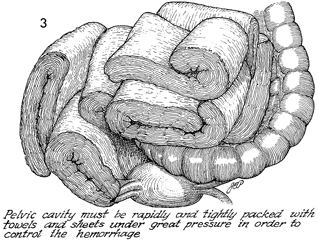
If the hemorrhage cannot be controlled with
the usual techniques and the patient has lost more then 5000
mL of blood, hypovolemic shock will result. The most efficacious
procedure in this situation consists of packing the pelvis, admission
of the patient to the surgical intensive care unit, and return
of the patient to the operating room in 48 hours. The rectus
fascia should not be closed; the skin should be closed with towel
clips.
In 48 hours, she can be returned
to the operating room with the proper vascular surgery team and
instruments. The towel clips can be removed from the skin, the
abdomen can be opened, packing can be removed, and in most cases,
the hemorrhage is contained. Occasionally, small bleeding points
can be oversewn or overligated. |
|
|