|
||||||
Malignant
Disease: Staging
of Gynecologic Application
of Vaginal Application
of Uterine Afterloading Applicators Abdominal
Injection of Chromic Phosphate Radical
Vulvectomy Reconstruction
of the Transverse
Rectus Colonic
"J" Pouch Rectal Ileocolic Continent Urostomy (Miami Pouch) Construction
of Neoanus Skin-Stretching
System Versus Skin Grafting Gastric
Pelvic Flap for Control
of Hemorrhage in Gynecologic Surgery Repair
of the Punctured Ligation
of a Lacerated Hemorrhage
Control in Presacral
Space What
Not to Do in Case of Pelvic Hemorrhage |
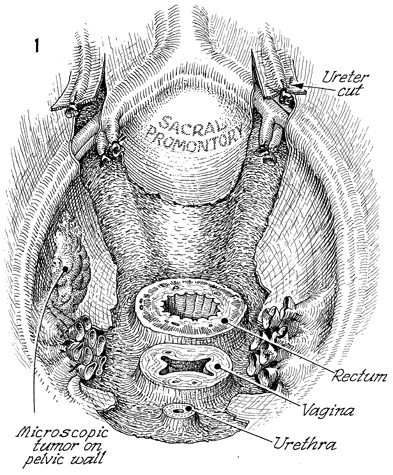
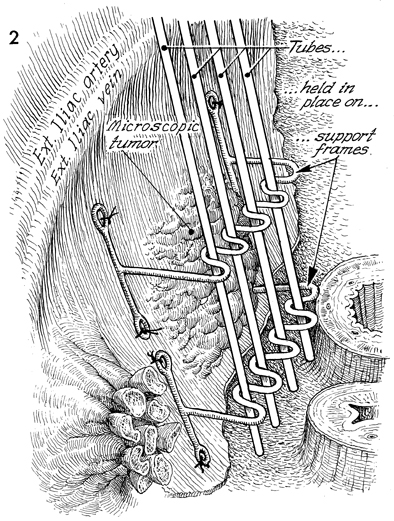
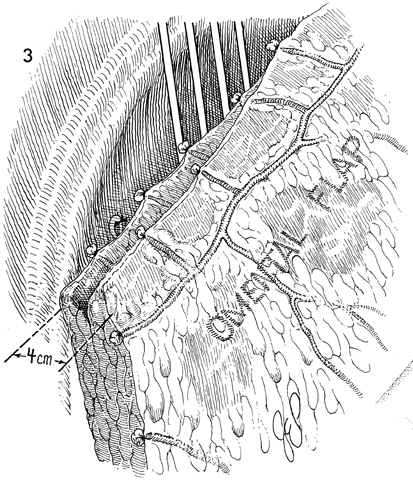
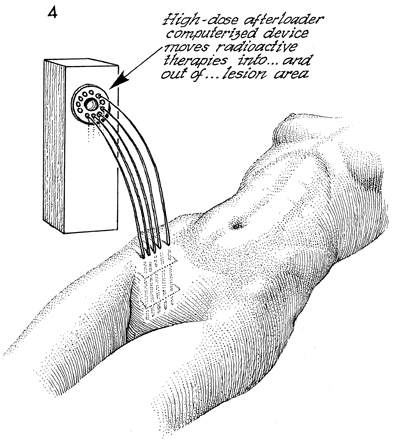
Pelvic High-Dose Afterloader If, at the time of total pelvic exenteration, tumor margins are close to the pelvic wall or if microscopic tumor remains on the pelvic wall in the area of radical excision of the pelvic wall, it is recommended that the tumor bed be irradiated even if the patient has already received total pelvic irradiation and intracavitary radiation therapy. Physiologic Changes. After total pelvic irradiation at 5000 cGy plus intracavitary radiation sources, either intracavitary radiation therapy with tandem and ovoid or high-dose afterloader techniques, the tumor on the pelvic wall frequently has not received enough irradiation to destroy it. In fact, the pelvic wall frequently receives no more than 5600 cGy in most techniques. Thus after total pelvic exenteration, there may be additional microscopic tumor present. It would be extremely difficult and dangerous to give more external beam therapy to the pelvic wall, and because of the inverse square law, there would be no method of giving standard tandem and ovoid therapy in the vagina that would significantly reach the pelvic wall. Therefore, if, following total pelvic exenteration, microscopic tumor remained on the pelvic wall, the high-dose afterloader technique could be used through a standard support frame device to give an additional cytoreductive dose of radiation to the tumor. Points of Caution. The destructive effect of radiation on the external iliac artery and vein and the possibility of radiation osteomyelitis to the ischial bones of the pelvis must be considered. In addition, the radiation should be covered by omental flaps or a rectus abdominal flap to give greater distance from the high-dose afterloader tubes in order not to damage adjacent intestine and allow neoangiogenesis to revascularize the pelvic wall. Technique
|
|||||
Copyright - all rights reserved / Clifford R. Wheeless,
Jr., M.D. and Marcella L. Roenneburg, M.D.
All contents of this web site are copywrite protected.