
![]()
Bartholin's Gland Cyst Marsupialization
Excision of Vulvar Skin, with Split-Thickness Skin Graft
Vaginal Outlet Stenosis Repair
Closure of Wide Local Excision of the Vulva
Wide Local Excision of the Vulva, With Primary Closure or Z-plasty Flap
Alcohol Injection of the Vulva
Cortisone Injection of the Vulva
Excision of the Vulva by the Loop Electrical Excision Procedure (LEEP)
Merring Operation
A small number of perineal pruritus (vulva and perianal) are persistent and not amenable to therapy by steroid cream and simple denervation by alcohol injection. Both of the above treatments should be given thorough trials before proceeding to the Merring operation, a more radical method of denervation. For some patients, no other remedy exists for this debilitating and embarrassing condition except surgical denervation of the vulva
The object of the operation is to transect the ilioinguinal nerve as it crosses into the mons pubis, the genital branch of the genitofemoral nerve, the cutaneous branches of the posterior femoral cutaneous nerve, and the labial branches of the pudendal nerve.
Pathophysiologic Changes: Transection and ligation of the cutaneous branches of the ileoinguinal genital femoral, posterior femoral and pudendal nerves denervates the vulva. Denervation blocks the sensation of itching. The absence of itching prevents scratching. The absence of scratching blocks the recurrent microlacerations that become inflamed and infected producing more itching and the vicious cycle of more scratching. Thus the denervated vulva is allowed to heal.
Points of Caution: Incomplete hemostasis is the major factor associated with morbidity in this operation. The branches of the pudendal nerve must be adequately ligated.
The wound should be adequately drained with suction drains.
Prophylactic coverage with antibiotics is indicated.
Technique
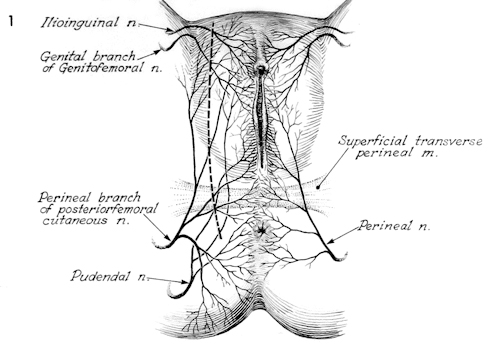
The nerve supply to the vulva is shown as well as the line of excision required to completely transect each nerve branch and produce a denervated vulva.
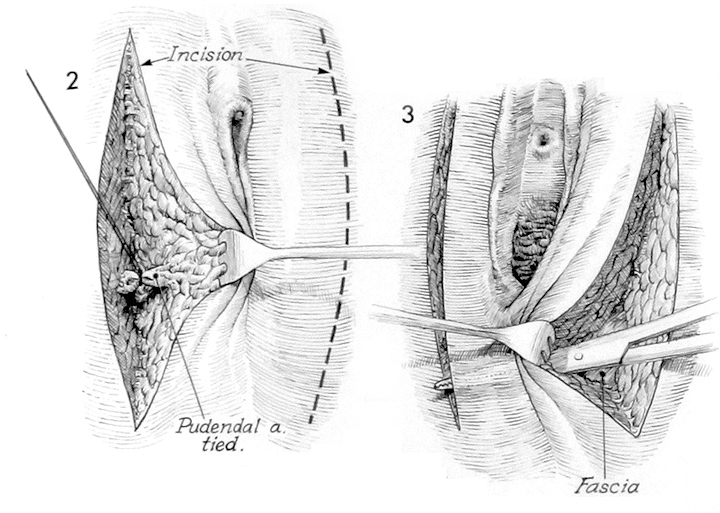
The patient is placed in a dorsal lithotomy position. The perineum is prepped and draped and the outline of the incision is made over the vulva with a surgical marker. The incision should extend from the mons pubis above the suspensory ligament of the clitoris over the lateral curvature of the labia majora to a level lateral to the anus. A similar incision is made on the opposite side.
The incision must be carried down to the fascia. The pudendal artery must be identified and ligated at 3 and 9 o’clock on each side of the vulva. When the fascia has been reached, a Kelly clamp is inserted on the top of the superficial transverse perineal muscle and is passed from one incision to the other taking care to avoid injury to the rectum.
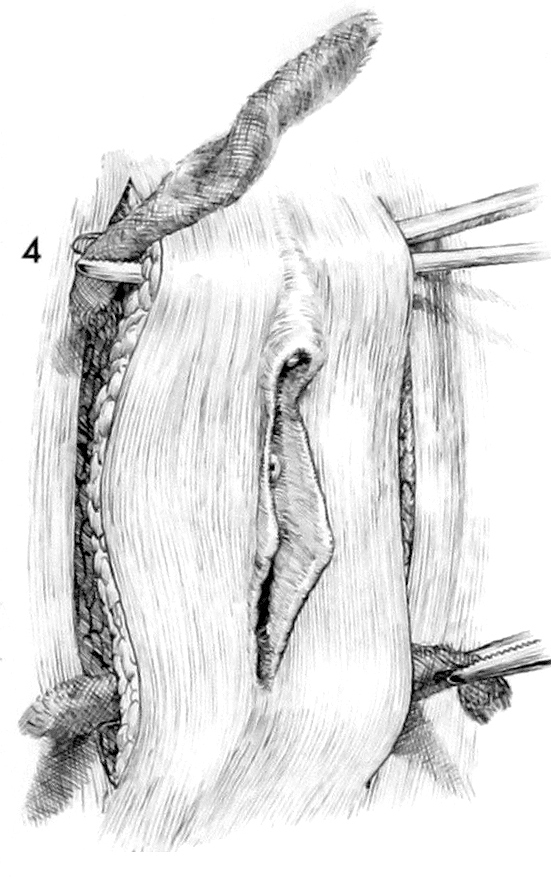
A sponge is brought through the incision from one side to the other beneath the vaginal mucosa and above the rectum. The incision must be carried all the way to the fascia in order to transect all the cutaneous nerve branches supplying the vulva. A Kelly clamp is passed underneath the suspensory ligament of the clitoris on top of the fascia and a sponge is likewise passed through this incision. The nerves supplying the vulva have been transected. The blood supply to the vulva is now dependent on the vascular plexus in the mons pubis and the hemorrhoidal plexus of the rectum. This blood supply should be adequate to prevent ischemia and necrosis of the vulva.
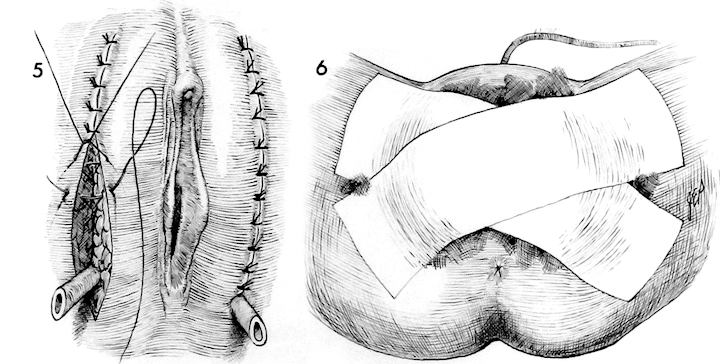
Closed suction drains are placed in the wound and brought out inferiorly. The incision is closed with interrupted 3/0 Prolene sutures.
A suprapubic Foley catheter can be inserted and a pressure dressing is placed over the vulva. The pressure dressing is left in place for 4 days. The patient is treated with prophylactic antibiotics. The suprapubic Foley catheter is removed on the 5th postoperative day. It is not uncommon for cellulitis and edema to remain in the perineum for 7 to 10 days. The drains are progressively advanced and removed when drainage is no longer present.
The cessation of itching in the perineum is dramatic, and frequently patients note that they have had the first full night of sleep without constant perineal itching in many months.