Vagina
and Urethra
Anterior Repair and Kelly
Plication
Site Specific Posterior Repair
Sacrospinous
Ligament Suspension of the Vagina
Vaginal Repair of Enterocele
Vaginal Evisceration
Excision of
Transverse Vaginal Septum
Correction of
Double-Barreled Vagina
Incision
and Drainage of Pelvic Abscess via the Vaginal Route
Sacral Colpoplexy
Le Fort Operation
Vesicovaginal Fistula
Repair
Transposition
of Island Skin Flap for Repair of Vesicovaginal Fistula
McIndoe Vaginoplasty
for Neovagina
Rectovaginal Fistula
Repair
Reconstruction of
the Urethra
Marsupialization
of a Suburethral Diverticulum by the Spence Operation
Suburethral
Diverticulum via the Double-Breasted Closure Technique
Urethrovaginal
Fistula Repair via the Double-Breasted Closure Technique
Goebell-Stoeckel
Fascia Lata Sling Operation for Urinary Incontinence
Transection
of Goebell-Stoeckel Fascia Strap
Rectovaginal
Fistula Repair via Musset-Poitout-Noble Perineotomy
Sigmoid
Neovagina
Watkins Interposition Operation |
Vesicovaginal Fistula Repair
Vesicovaginal fistulae are usually secondary to obstetrical trauma,
pelvic surgery, advanced pelvic cancer, or radiation therapy for treatment
of pelvic cancer.
The basic principles for treatment of vesicovaginal fistulae have
changed little since the mid-19th century work of Marion Sims. The
principles are (1) to ensure that there is no cellulitis, edema, or
infection at the fistula site prior to closing the fistula and (2)
to excise avascular scar tissue and approximate the various layers
of tissue broadside to broadside without tension. A 20th century addition
to these principles is that of using transplanted blood supply from
the vestibular fat pad, bulbocavernosus muscle, gracilis muscle, or
the omentum.
The type of suture used appears less significant when the above principles
are followed. In general, we have used the glycolic acid sutures such
as Dexon or Vicryl because of their reabsorption and reduced tissue
reaction. Many surgeons prefer, however, to use a non-absorbable monofilament
suture of nylon or Prolene on the vaginal mucosa. These sutures should
not be placed into the bladder mucosa. If they are left in the bladder
for long periods of time, urinary stone formation will occur.
The purpose of the operation is to close the vesicovaginal fistula
permanently without encroaching on the ureter or the urethral orifices.
Physiologic Changes. The fistula is closed, and resumption
of micturition via the urethra resumes.
Points of Caution. Adequate blood supply to the tissue
surrounding the fistula must be provided. Excision of scar tissue is
vital to closure. Recently, tissue transplants have been used to bring
in external blood supply to the fistula site. This is a vital point
when the fistula is secondary to radiation therapy. In addition, when
the fistula is secondary to radiation therapy, we have performed a
temporary urinary diversion by ileal loop. This has dramatically improved
our ability to permanently close radiation fistulae. At a subsequent
operation, the ileal loop can be reimplanted in the dome of the bladder
after the fistula has been closed and bladder function is adequate.
In all fistulae, the principle of dual drainage is vital for proper
closure. A transurethral as well as suprapubic Foley catheter is left
in place until the fistula has closed. Generally, the transurethral
catheter is removed after 2 weeks, but the suprapubic catheter is left
in place for at least 3 weeks. Acidification of the urine with ascorbic
acid or cranberry juice is helpful in reducing urinary tract infection.
Frequent urine culture and appropriate antibiotic therapy are indicated,
however.
If an alkaline urine is present with a vesicovaginal
fistula, the urine will precipitate triple-sulfate crystals and deposit
them on the opening of the vagina.
These are quite painful and must
be completely removed prior to closure.
Technique
For vesicovaginal fistula closure
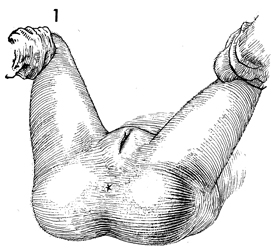
the patient is placed in the dorsal lithotomy position. The vulva
and vagina are prepped and draped. |
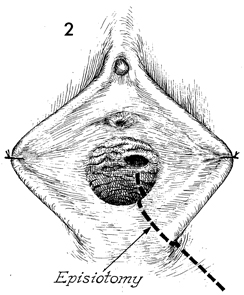
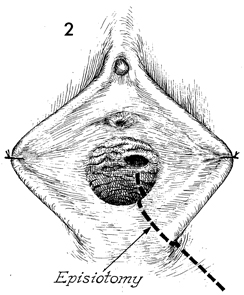
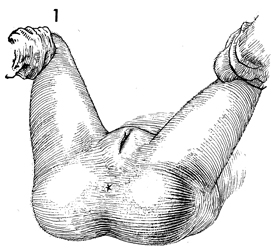
Adequate exposure of the fistula
must be made. Many unsuccessful fistula closures have resulted
from the failure to achieve adequate exposure of the fistula
site, poor placement of the sutures, and closure of the fistula
under tension. A large mediolateral episiotomy is frequently
required and should be carried up to the area of the fistula. |
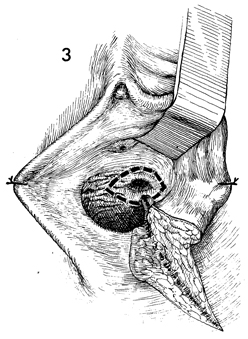
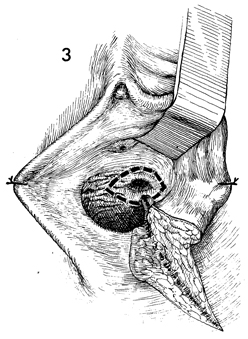
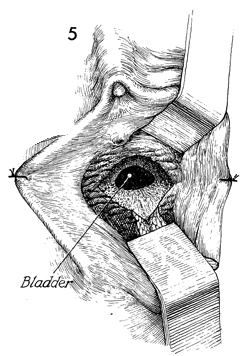
With adequate exposure the fistula
tract can be excised with a scalpel. The incision is carried
around the circumference of the fistula. |
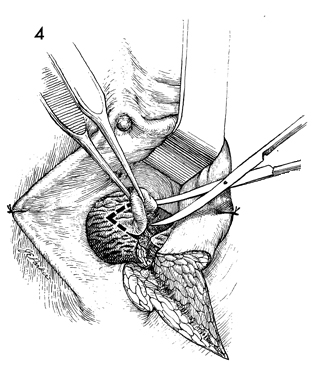
The margin of the fistula tract
is elevated with thumb forceps and excised with Metzenbaum scissors.
The entire tract is dissected. Frequently, when dense scar tissue
has been released, the fistula will be 2-3 time larger than noted
preoperatively. |
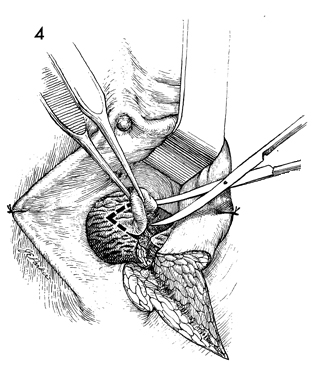
The layers of the bladder wall and
vagina should be adequately delineated, and each of these layers
should be mobilized to allow the layers to be drawn together
with fine sutures without tension. |
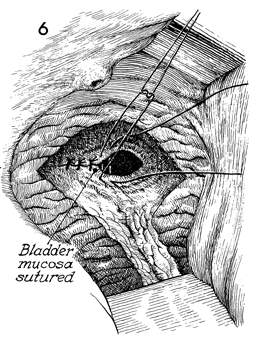
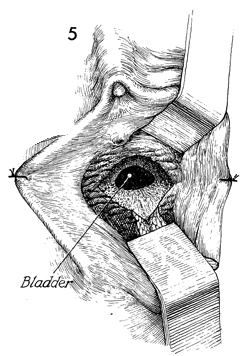
The bladder mucosa is identified and
closed with interrupted 4-0 synthetic absorbable suture. An attempt
should be made to keep the suture in the submucosal layer. We do
not perform running locking sutures or continuous suture, since
we feel this reduces the blood supply that is vital to proper closure. |
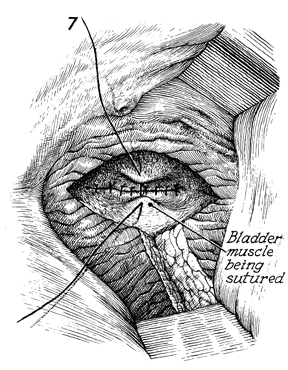
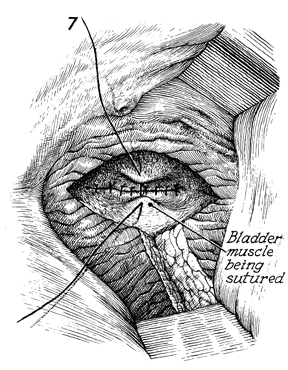
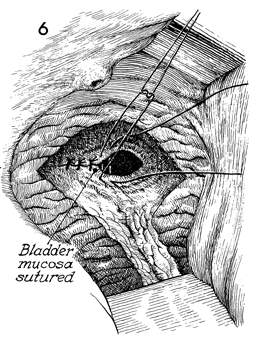
A second layer, the bladder
muscle, is closed with 2-0 synthetic absorbable suture. |
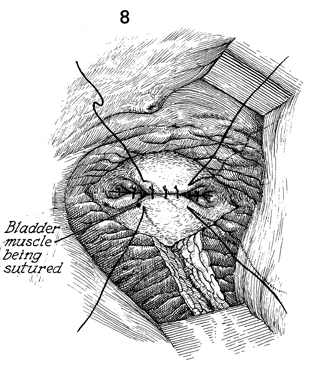
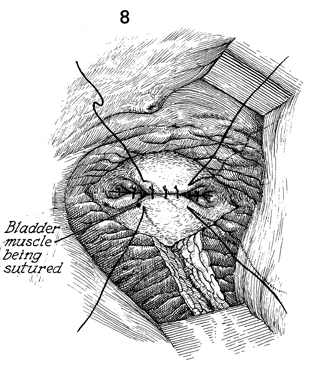
The bladder muscle is completely closed
over the fistula area with interrupted 2-0 synthetic absorbable
suture. |
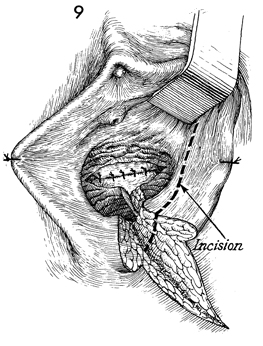
At this point, it is necessary
in high-risk cases to seek an external blood supply for the
fistula site. This can be the bulbocavernosus muscle from beneath
the labia majora, or in cases where a large fistula exists
or where the fistula is high in the vaginal canal, the gracilis
muscle from the leg or the rectus abdominis muscle can be brought
in to cover the fistula site.
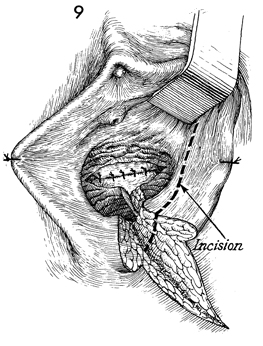
If the bulbocavernosus is
selected, two incision sites are acceptable. One is on the
inside of the labia minora as seen in Figure 9. The other is
down the body of the labia majora. If the latter incision is
selected, the bulbocavernosus muscle must be tunneled under
the labia minora into the episiotomy wound. |
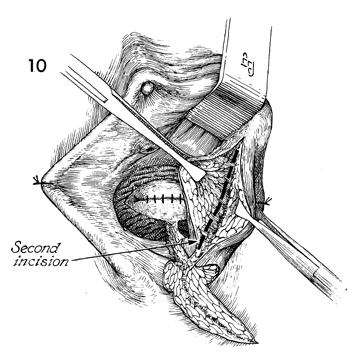
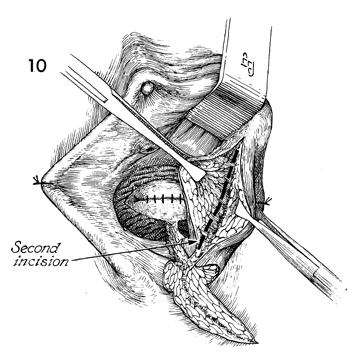
Allis clamps are used for retraction
of the labia, and a scalpel is used for dissection down to the
bulbocavernosus muscle. It is important to enlarge the incision
so that the entire muscle can be visualized. |
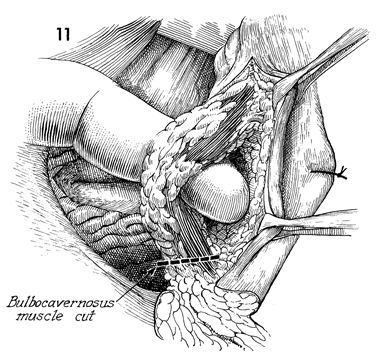
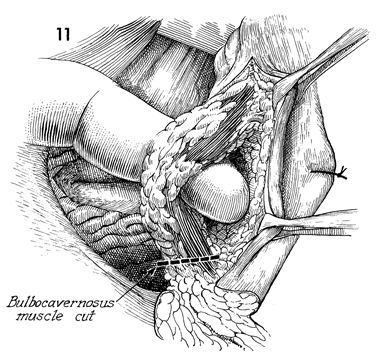
The bulbocavernosus muscle is identified
and mobilized. Frequently, at the level indicated here, the
branches of the pudendal artery and vein enter the muscle and
may have to be clamped and ligated for hemostasis. The bulbocavernosus
muscle should be mobilized by blunt and sharp dissection up
to the level of the clitoris and transected at its insertion
in the perineal body. |
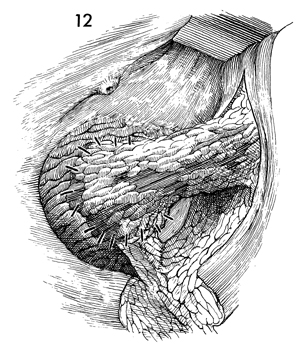
If the initial incision has been made
on the inside of the labia minora, no tunneling of the bulbocavernosus
muscle is needed, and the muscle is swung into position, covering
the fistula site. It is sutured to the perivesical tissue with
interrupted 3-0 synthetic absorbable sutures. If the initial incision
has been carried over the labia majora, a tunnel is created with
a Kelly clamp under the labia minora into the episiotomy incision.
The bulbocavernosus muscle is pulled through this tunnel, applied
to the fistula site, and sutured into place with interrupted 3-0
synthetic absorbable suture. |

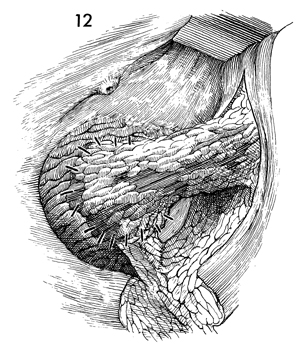
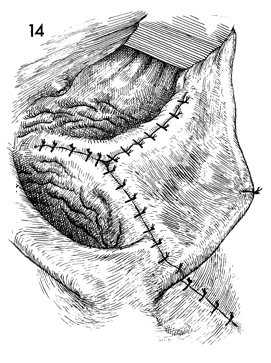
The vaginal mucosa must be mobilized
for closure without tension. Generally, the wound is closed with
interrupted 0 synthetic absorbable suture. |
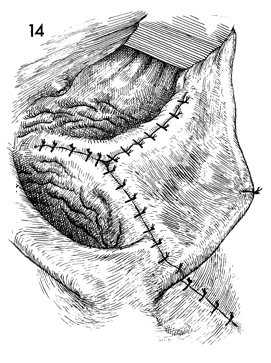
The vaginal incision, the episiotomy
incision, and the incision for the bulbocavernosus muscle transplant
are closed. |
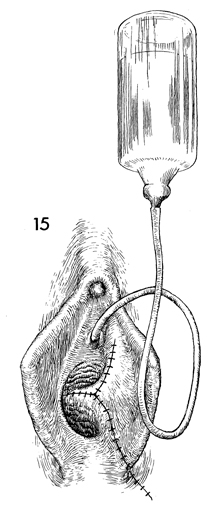
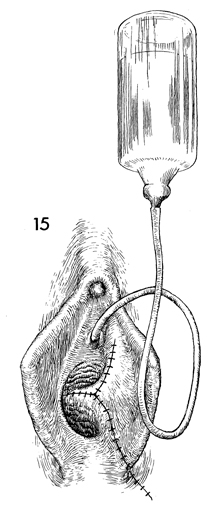
A Foley catheter is inserted
through the urethra. The bladder is generally filled with approximately
200 mL of methylene blue or sterile milk solution to ascertain
if the fistula is completely closed. We frequently perform this
same procedure after Steps 7 and 8 to demonstrate complete closure
of the fistula site.
In addition to the transurethral
Foley catheter, a suprapubic Foley catheter is placed as demonstrated
in Bladder and Ureter. Dual drainage for the fistula closure is vital. |
|
|