Vagina
and Urethra
Anterior Repair and Kelly
Plication
Site Specific Posterior Repair
Sacrospinous
Ligament Suspension of the Vagina
Vaginal Repair of Enterocele
Vaginal Evisceration
Excision of
Transverse Vaginal Septum
Correction of
Double-Barreled Vagina
Incision
and Drainage of Pelvic Abscess via the Vaginal Route
Sacral Colpoplexy
Le Fort Operation
Vesicovaginal Fistula
Repair
Transposition
of Island Skin Flap for Repair of Vesicovaginal Fistula
McIndoe Vaginoplasty
for Neovagina
Rectovaginal Fistula
Repair
Reconstruction of
the Urethra
Marsupialization
of a Suburethral Diverticulum by the Spence Operation
Suburethral
Diverticulum via the Double-Breasted Closure Technique
Urethrovaginal
Fistula Repair via the Double-Breasted Closure Technique
Goebell-Stoeckel
Fascia Lata Sling Operation for Urinary Incontinence
Transection
of Goebell-Stoeckel Fascia Strap
Rectovaginal
Fistula Repair via Musset-Poitout-Noble Perineotomy
Sigmoid
Neovagina
Watkins Interposition Operation |
Suburethral Diverticulectomy via the Double-Breasted
Closure Technique
Suburethral diverticula may be discovered in patients evaluated for
recurrent or chronic urinary tract infections. The diverticula formation
can be congenital or secondary to trauma of the female urethra.
The purpose of the operation is to remove the diverticulum
and close the urethra without producing a stricture. This procedure
should be utilized only for diverticula located in the middle and proximal
thirds of the urethra. Suburethral diverticula in the distal one-third
of the urethra are managed effectively by the Spence operation.
Physiologic Changes. A source of chronic infection
that is also a potential site of urethral stone formation is removed.
Points of Caution. After excision of the suburethral
diverticulum, adequate mobilization of the surrounding tissues must
be made to close the wound without tension and reduce the chance of
urethral stricture. If the tissue is brought together under tension,
necrosis can occur, and a fistula may develop.
Technique
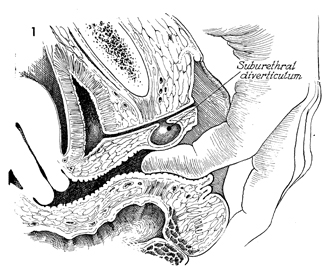
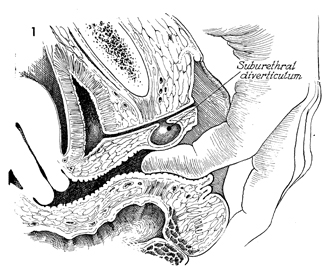
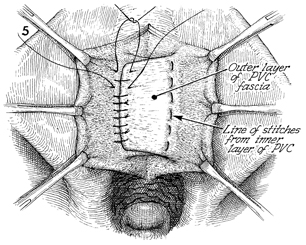
Figure 1 is a sagittal section of
the female bladder, urethra, and vagina, showing a suburethral
diverticulum. Diverticula can be diagnosed either by urethroscopy
or with the use of a Davis double-balloon catheter in which x-ray
contrast media is injected under pressure.
This special catheter entraps x-ray
contrast dye between the two inflated balloons, forcing dye into
a diverticulum. A lateral x-ray film can demonstrate the diverticulum. |
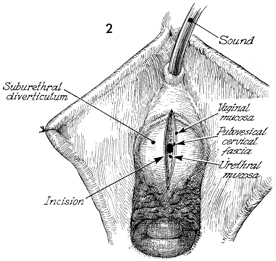
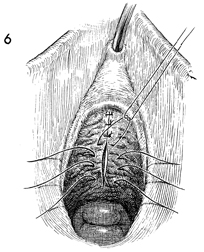
The patient is placed in the dorsal
lithotomy position, and the perineum is prepped and draped in
the usual fashion. A uterine sound has passed through the urethra
into the bladder. The vaginal mucosa is opened over the suspected
diverticulum. Figure 2 shows the vaginal mucosa, pubovesical
cervical fascia, and the urethral mucosa. |
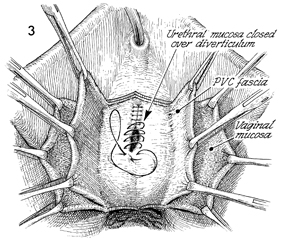
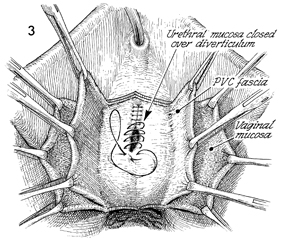
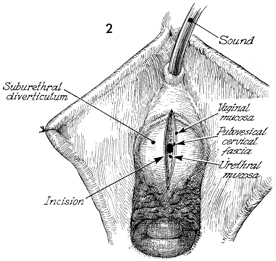
The urethral mucosa is closed over
the diverticulum with a running monofilament 4-0 synthetic absorbable
suture. The sutures should be placed with the uterine sound in
position to prevent stricture of the urethra. Notice that the
pubovesical cervical (PVC) fascia has been developed
into 2-3 cm-wide flaps of fascia. The vaginal mucosa has been
dissected laterally and is held laterally with Allis clamps. |
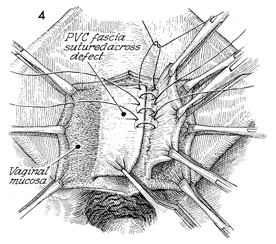
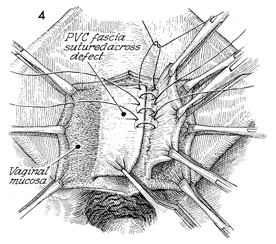
The double-breasted closure technique
is performed with monofilament delayed synthetic absorbable suture.
The right pubovesical cervical fascia flap is sutured across
to the base of the opposite pubovesical cervical fascia flap.
It is best to place all these sutures prior to tying them. This
will allow more accurate placement of the sutures.
Note that the vaginal mucosa is
retracted laterally. On the patient's left, the opposite pubovesical
cervical fascia is retracted out of the suture line. |
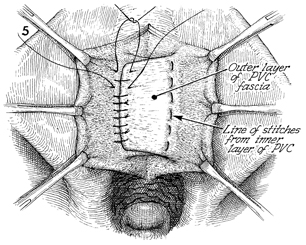
The left pubovesical cervical fascia
flap is now sutured over the right pubovesical cervical fascia
flap in a double-breasted fashion with monofilament delayed synthetic
absorbable suture used. |
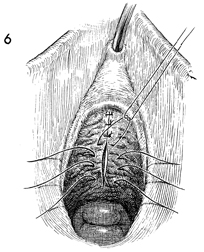
The vaginal mucosa is closed in the
midline with 2-0 synthetic absorbable suture. Catheter drainage
should be continuous for 1 week. This can be accomplished with
a suprapubic Foley catheter or a transurethral Foley catheter. |
|