Vagina
and Urethra
Anterior Repair and Kelly Plication
Site Specific Posterior Repair
Sacrospinous Ligament Suspension of the Vagina
Vaginal Repair of Enterocele
Vaginal Evisceration
Excision of Transverse Vaginal Septum
Correction of Double-Barreled Vagina
Incision and Drainage of Pelvic Abscess via the Vaginal Route
Sacral Colpoplexy
Le Fort Operation
Vesicovaginal Fistula Repair
Transposition of Island Skin Flap for Repair of Vesicovaginal Fistula
McIndoe Vaginoplasty for Neovagina
Rectovaginal Fistula Repair
Reconstruction of the Urethra
Marsupialization of a Suburethral Diverticulum by the Spence Operation
Suburethral
Diverticulum via the Double-Breasted Closure Technique
Urethrovaginal Fistula Repair via the Double-Breasted
Closure Technique
Goebell-Stoeckel Fascia Lata Sling Operation for Urinary Incontinence
Transection of Goebell-Stoeckel Fascia Strap
Rectovaginal Fistula Repair via Musset-Poitout-Noble Perineotomy
Sigmoid
Neovagina
Watkins Interposition Operation
|
Anterior Repair and Kelly Plication
Anterior repair is used for correction of a cystourethrocele. It can
be combined with Kelly plication of the urethra when, in addition to
a cystourethrocele, the patient is experiencing stress incontinence
of urine.
The purpose of the anterior repair is to reduce the cystourethrocele
and reinforce the pubovesical cervical fascia support of the bladder
and urethra. The purpose of the Kelly plication of the urethra is to
reduce the diameter of the urethra.
Physiologic Changes. In
the Kelly plication, the surgeon increases the intraurethral pressure
to a level higher than the intravesical pressure in the resting and
stress state, i.e., with a Valsalva maneuver. When the patient tries
to void, however, the detrusor contractions reverse the pressure
relationship so that the intravesical pressure exceeds the intraurethral
pressure.
Points of Caution. Care must be taken to
dissect the anterior vaginal mucosa off the pubovesical cervical
fascia without carrying the dissection beneath the fascia. The depth
of penetration of the plication suture must be controlled; the purpose
is to plicate the fascia, not the urethra. Excessive amounts of mucosa
should not be removed to avoid unduly reducing the volume of the
vagina.
Technique
|
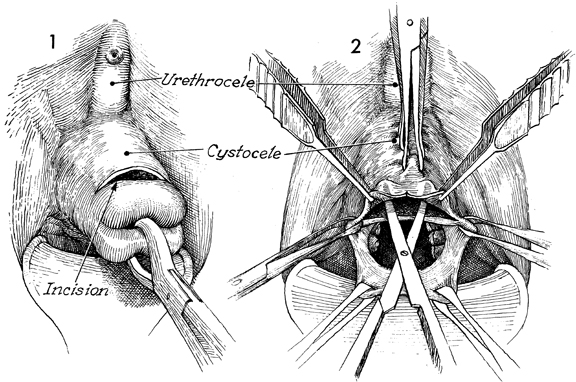
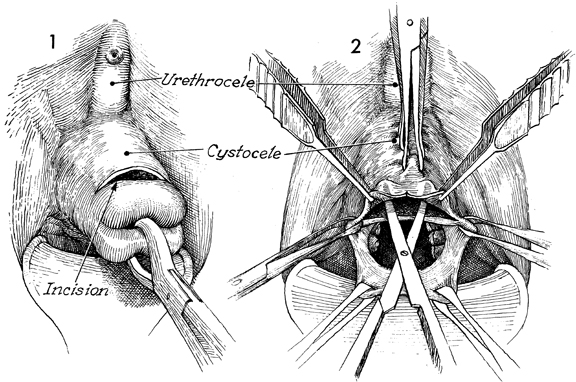
The patient is placed in the dorsal lithotomy
position. The perineum, vulva, and vagina are surgically prepared.
The anterior repair can be performed with the uterus in place
or after it has been removed. The technique is the same. The
urethrocele and cystocele are shown. A transverse incision is
made at the junction of the vaginal mucosa and cervix. This incision
should be carried down to the pubovesical cervical fascia while
the cervix is held on traction with a Jacobs tenaculum. |
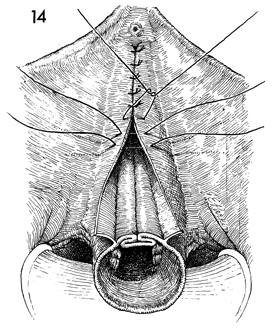
The uterus has been removed. The lateral
edges of the vaginal cuff are held with Allis clamps on tension.
Several Allis clamps are placed 3-4 cm apart up the midline of
the anterior vaginal wall. The vaginal mucosa itself is held
with thumb forceps and, with curved Mayo scissors, is undermined
for approximately 3-4 cm up to the first of the Allis clamps
placed in the midline. It is important for the assistant to hold
the three Allis clamps in the immediate area of dissection on
tension, creating a triangle. This will assist the surgeon in
keeping the dissection in the proper plane between vaginal mucosa
and pubovesical cervical fascia. |
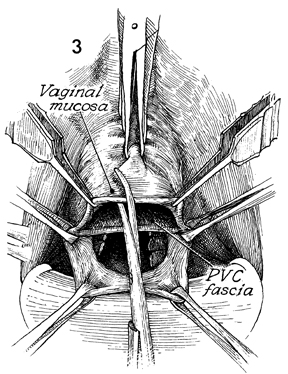
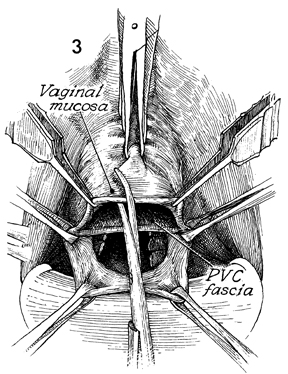
When the vaginal mucosa has been dissected
off the pubovesical cervical (PVC) fascia, it is opened with
scissors in the midline. |
The procedure in Step 3 is
repeated after wide Allis clamps have been applied to the edges
of the vaginal mucosa. |
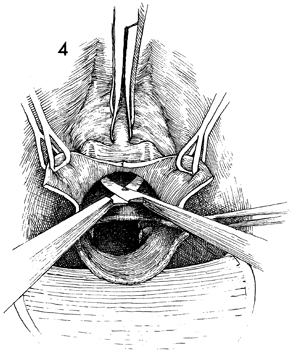
The vaginal mucosa is opened in the midline
up to the next Allis clamp. This is continued until the vagina
is opened to within 1 cm of the urethral meatus. As the vagina
is opened, the edges of the mucosa are grasped with wide Allis
clamps and held in the lateral position by the assistants. |
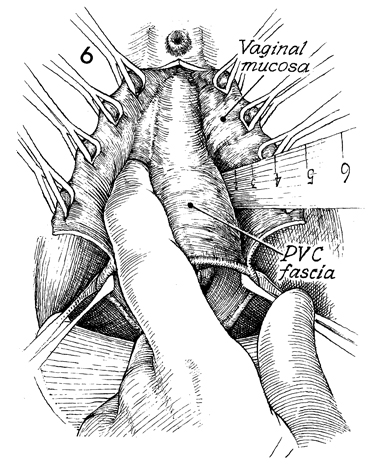
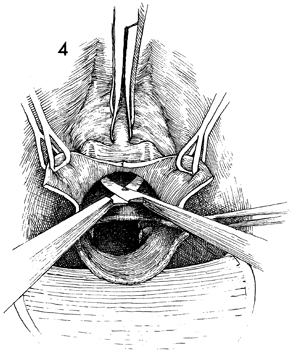
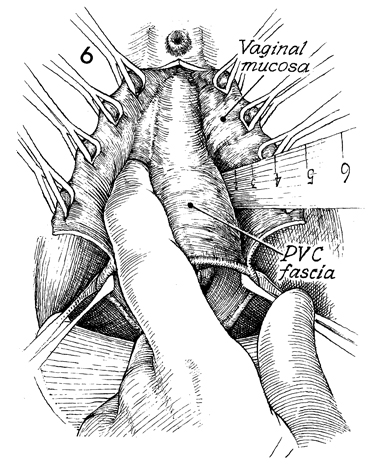
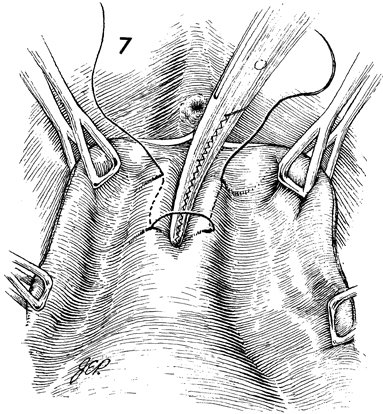
The pubovesical
cervical (PVC) fascia is separated from the vaginal mucosa. The
surgical assistants maintain tension on the wide Allis clamps
to form an opening like a "Chinese fan." Scalpel, scissors, or
blunt dissection can be used to remove the fascia from the vaginal
mucosa. It is helpful to start the dissection with a scalpel,
cutting the pubovesical cervical fascia at the edge of the vaginal
mucosa and dissecting it downward with the finger or the handle
of the scalpel. This dissection should be continued until the
bladder and urethra are separated from the vaginal mucosa and
are clearly identified and the urethral vesical angle has been
ascertained. |
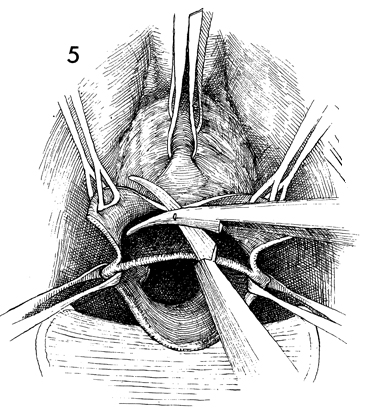
If the patient has stress incontinence of
urine and needs a Kelly plication, the first mattress suture
is placed in the wall of the urethra approximately 1 cm below
the urethral meatus. Traditionally, a nonabsorbable suture has
been used for the plication. The suture, 1 cm in length, should
be placed along the lateral margin of the urethra. When the suture
is completed, a curved Kelly clamp is held in position to invert
the urethral tissue as the suture is tied. |
Additional Kelly plication sutures are placed. |
The last Kelly plication suture is placed
approximately 2 cm beyond the urethral vesical angle. |
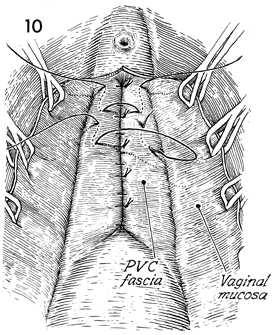
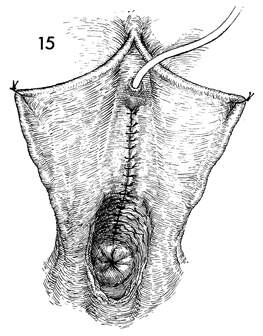
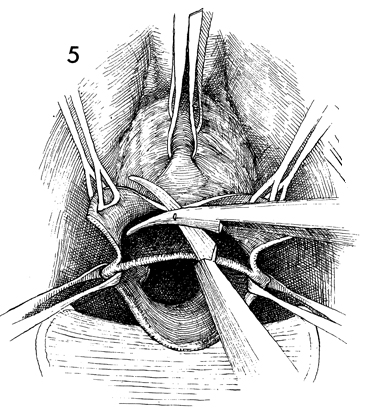
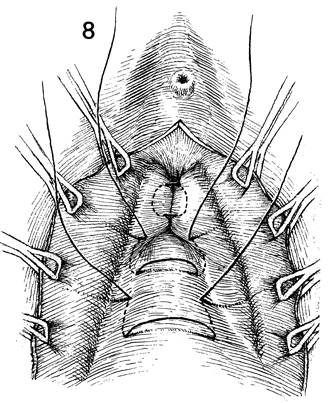
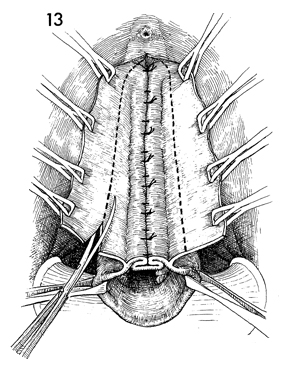
The anterior repair is started by placing
0 synthetic absorbable sutures in the pubovesical cervical (PVC)
fascia, starting at the level of the first Kelly plication suture
or 1 cm below the urethral meatus. The suture should be placed
only in the pubovesical cervical fascia, not in the bladder wall. |
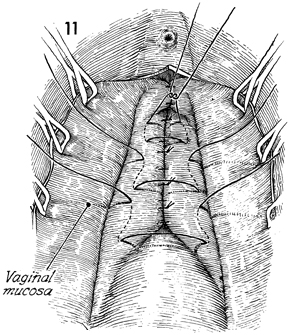
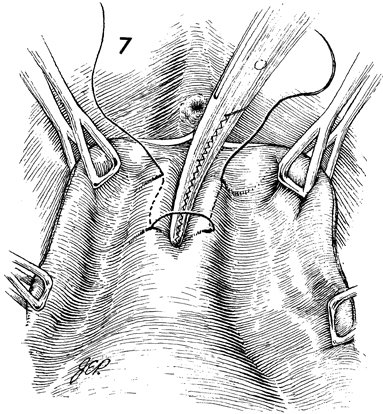
The edges of the vaginal mucosa are retracted
laterally with Allis clamps. The remaining pubovesical cervical
fascia is plicated in the midline with multiple interrupted 0
absorbable mattress sutures. |
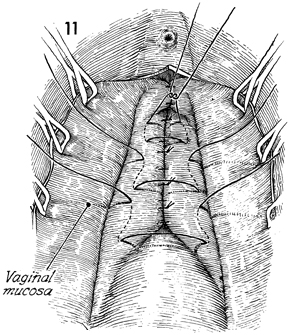
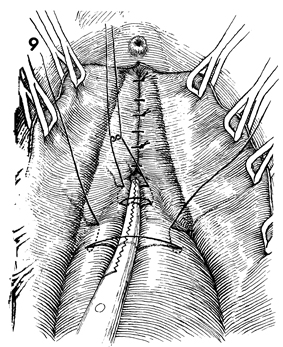
The plication of the pubovesical cervical
fascia should continue until the entire cystourethrocele has
been reduced. |
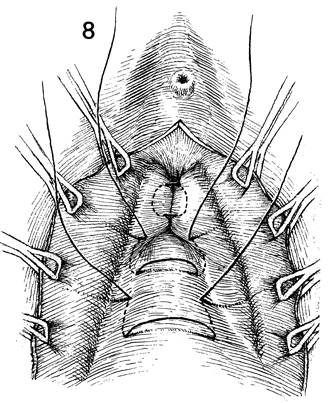
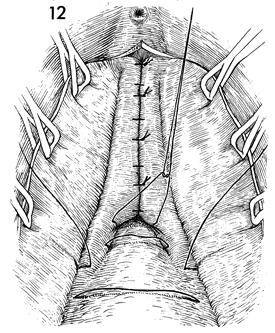
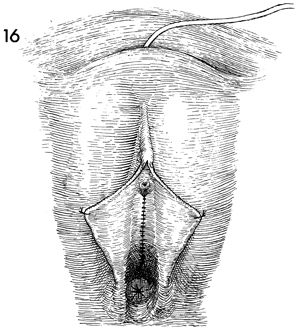
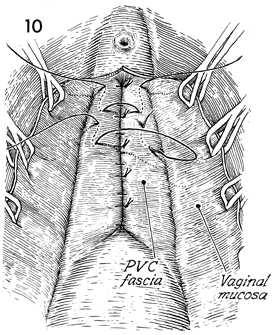
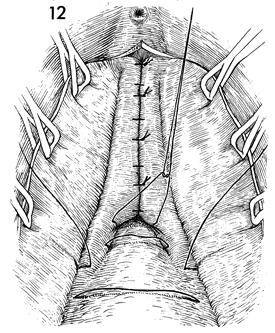
The edges of the vaginal mucosa are held
on tension. The excessive vaginal mucosa is trimmed away. The
lower portion of the drawing shows a cross section of vaginal
cuff and plicated pubovesical cervical fascia. |
The vaginal mucosa is sutured in the midline
with interrupted 0 synthetic absorbable suture down to the vaginal
cuff. The edge of the vaginal cuff is sutured with a running
0 absorable suture and left open. |
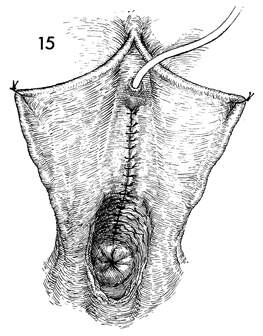
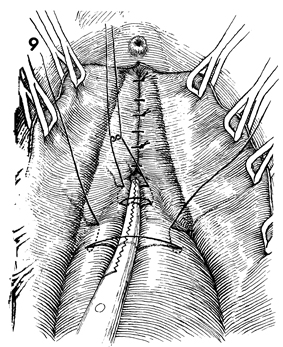
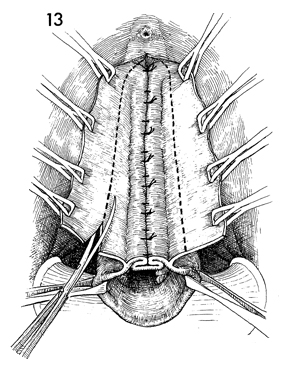
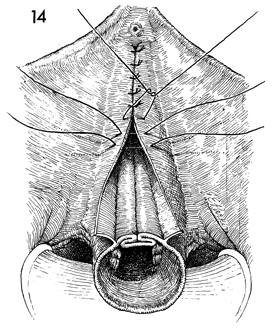
The completed anterior repair and Kelly plication
with the sutured anterior vaginal mucosa is shown. The sutured
but open vaginal cuff is seen. A Foley catheter is inserted transurethrally. |
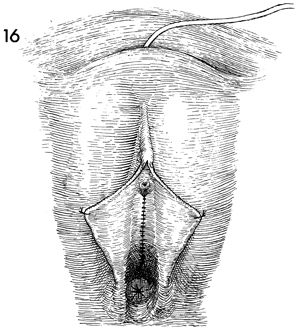
An alternative method of bladder
drainage is the suprapubic insertion of a Foley catheter (see
Bladder and Ureter). |
|