|
||||||
Anterior Repair and Kelly
Plication |
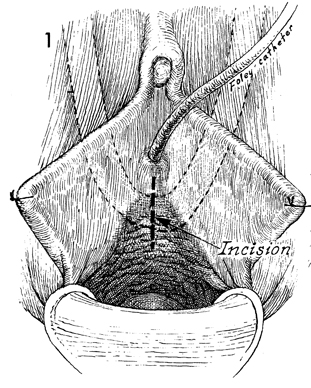
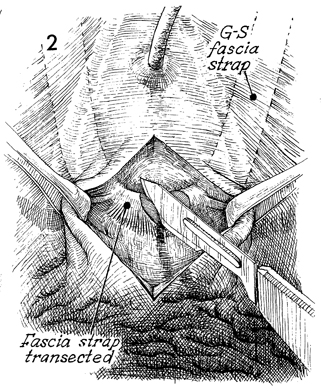
Transection of Goebell-Stoeckel The most serious drawback of the Goebell-Stoeckel fascia lata sling operation for restoration of urinary continence is the complication of postoperative urinary retention. In most cases, this results from the surgeon pulling the strap too tightly or from excessive contraction during healing, allowing the strap to pull itself too tightly. In general, the surgeon should allow 3 months before resorting to transection of the strap, since most cases of urinary retention are resolved with conservative therapy. The purpose of the operation is to transect the strap without entering the urethrovesical bladder mucosa. When the strap alone has been transected, it separates approximately 1-2 cm and is densely adherent to the lateral periurethral tissue. Physiologic Changes. With separation of the strap in the midline, the urethra is allowed to enlarge slightly. The intraurethral pressure is thereby reduced to a level that will allow the normal intravesical pressure on voiding to overcome the resistance in the urethra. The patient can then void and empty the bladder normally. Fortunately, in the majority of cases the dense adhesions of the strap to the lateral periurethral tissue continue to provide sufficient increase in the intraurethral pressure to avoid recurrent incontinence. Points of Caution. The strap should be carefully identified (1) prior to making the vaginal incision, so that only the vaginal mucosa is separated, and (2) prior to cutting into the pubovesical cervical fascia. Technique
|
|||||
Copyright - all rights reserved / Clifford R. Wheeless,
Jr., M.D. and Marcella L. Roenneburg, M.D.
All contents of this web site are copywrite protected.