Vagina
and Urethra
Anterior Repair and Kelly
Plication
Site Specific Posterior Repair
Sacrospinous
Ligament Suspension of the Vagina
Vaginal Repair of Enterocele
Vaginal Evisceration
Excision of
Transverse Vaginal Septum
Correction of
Double-Barreled Vagina
Incision
and Drainage of Pelvic Abscess via the Vaginal Route
Sacral Colpoplexy
Le Fort Operation
Vesicovaginal Fistula
Repair
Transposition
of Island Skin Flap for Repair of Vesicovaginal Fistula
McIndoe Vaginoplasty
for Neovagina
Rectovaginal Fistula
Repair
Reconstruction of
the Urethra
Marsupialization
of a Suburethral Diverticulum by the Spence Operation
Suburethral
Diverticulum via the Double-Breasted Closure Technique
Urethrovaginal
Fistula Repair via the Double-Breasted Closure Technique
Goebell-Stoeckel
Fascia Lata Sling Operation for Urinary Incontinence
Transection
of Goebell-Stoeckel Fascia Strap
Rectovaginal
Fistula Repair via Musset-Poitout-Noble Perineotomy
Sigmoid
Neovagina
Watkins Interposition Operation |
Rectovaginal Fistula Repair
Via Musset-Poitout-Noble Perineotomy
Rectovaginal fistula in developed countries is predominately secondary
to (1) gynecologic surgical procedures and (2) failed episiotomy repairs.
In less developed countries, a rectovaginal fistula is generally the
sequela from pressure necrosis of prolonged and obstructed labor.
Fistulae
secondary to cancer therapy (surgical or radiation induced) require
special techniques not required of rectovaginal fistulae associated
with benign gynecologic surgery, failed episiotomies, and obstetrical
delivery.
Modern surgical suture has a significant influence
on the successful closure of these fistulae. Woven suture products,
synthetic or nonsynthetic, are associated with microabscesses in the
fistula repair. Bacteria become entwined in the woven suture product,
and thus the suture product acts as a wick carrying bacteria to the
wound. With the use of monofilament synthetic absorbable suture, we
no longer return patients to the operating room on the eighth postoperative
day for removal of permanent sutures such as woven Mersilene and silk.
There is debate as to whether it is preferable to use monofilament
delayed synthetic absorbable suture or a synthetic rapidly absorbable
suture. Currently, we use the monofilament delayed synthetic absorbable
suture on all layers of the fistula repair. Suture abscesses have been
reduced. Therefore, until we have further data, we will continue to
use the monofilament delayed synthetic absorbable suture polydioxanone
rather than the monofilament synthetic absorbable suture poliglecaprone.
Physiologic Changes. The
main physiologic change after repair of a rectovaginal fistula is
to eliminate stool flowing from the rectum through the vagina. Concern
may exist for the competence and continuity of the transected and
reconstructed anal sphincter muscle. Transection of an otherwise
competent anal sphincter and careful and proper reconstruction with
suturing the fascia of the muscle should not be associated with incompetence
of the sphincter and fecal incontinence secondary to that incompetent
sphincter.
Points of Caution. Rectovaginal fistulae may present
as multiple fistulae in a so-called honeycomb appearance or as one
single fistula. It is important to excise the entire fistula tract
of all fistulae.
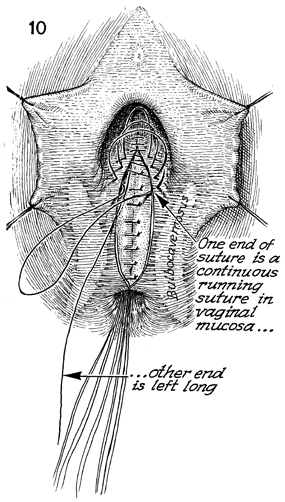
Technique
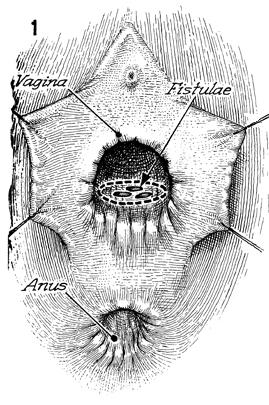
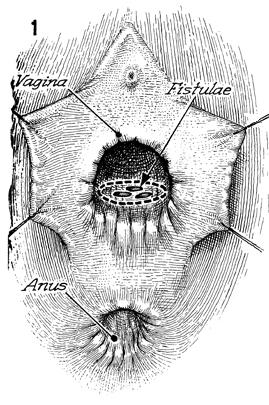
Figure 1 shows several rectovaginal
fistulae with a honeycomb appearance. An incision that encompasses
the entire fistulae should be made in the posterior vaginal wall
mucosa. |
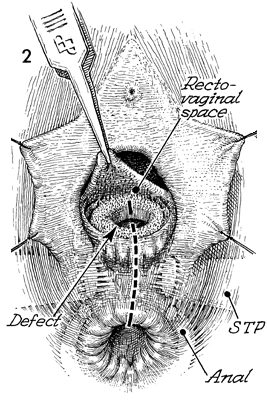
The fistula tract has been removed
down to the rectal mucosa. The margins of the vagina that remain
are elevated and mobilized with sharp dissection. A perineotomy
incision is made through the vagina, the superficial transverse
peritonea (STP), the anal sphincter, and anal mucosa. |

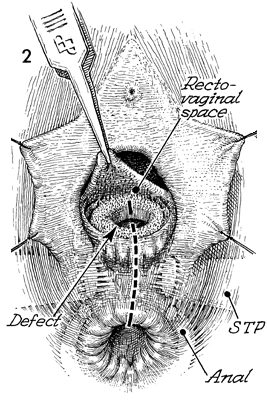
Figure 3 illustrates the surgical
removal of the fistulae, the perineotomy with the transected
anal sphincter, the transected superficial transverse peritonea,
and the rectovaginal space that has been developed surgically
between the vaginal mucosa and the rectum (R). |
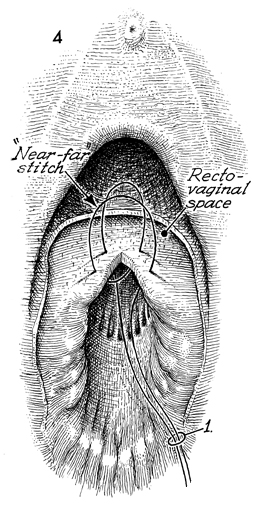
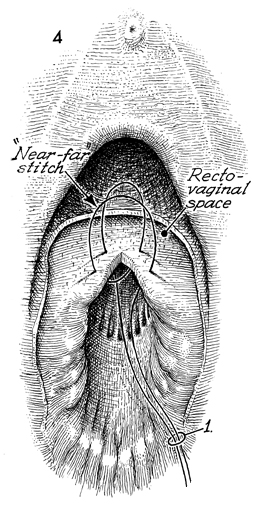
The rectum is repaired with a far-near-near-far
Connell inverting suture that inverts the mucosa into the lumen
of the rectum. Care is taken that the knot is tied in the rectum
to prevent the knot from becoming a wick for bacteria in this
area. |
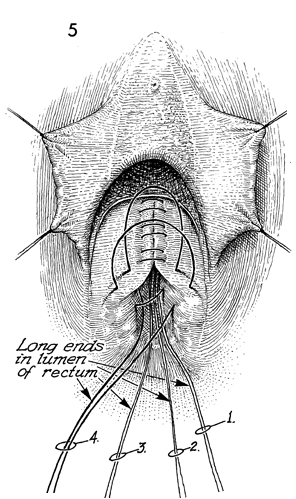
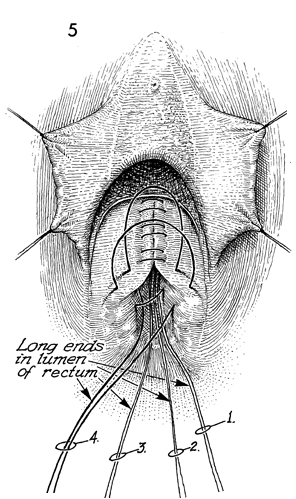
The rectum is repaired down to the anal mucosa;
the sutures are then cut. 1-5. |
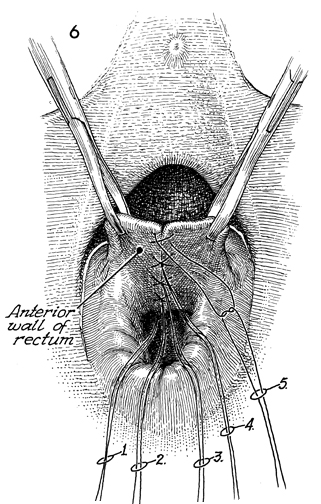
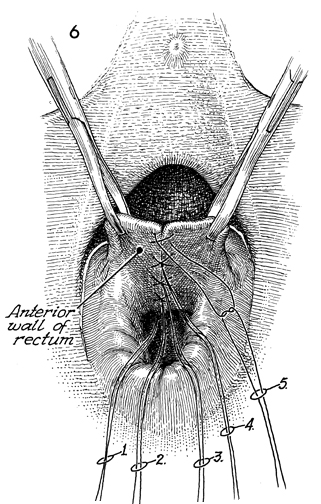
Figure 6 shows the anterior rectal wall with
far-near-near-far sutures in place. The excess suture outside
the knot can be cut. This differs from the traditional technique
where woven suture products were used, since the sutures had
to be left long so they could be removed from the wound on the
seventh postoperative day. After the rectal mucosa has been sutured,
a decision must be made to bring in an exterior source of blood
supply, such as the bulbocavernosus muscles with their vestibular
fat pad. If that is to be performed, it should be performed at
this point, and the bulbocavernosus muscle with its fat pad should
be sutured over the rectal suture line before beginning the posterior
repair with plication of the levator muscle in the midline. |
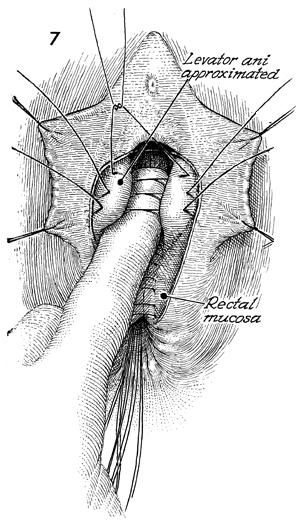
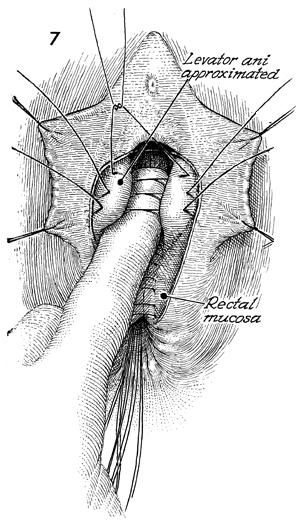
After the rectal mucosa has been sutured
closed, the finger of the left hand is placed on top of the rectal
suture line. This invagination produces prominence of the levator
ani muscles. Delayed synthetic absorbable suture is placed in
the levator muscles to plicate them on top of the rectal suture
line. |
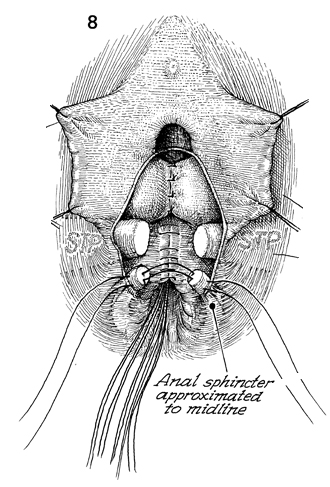
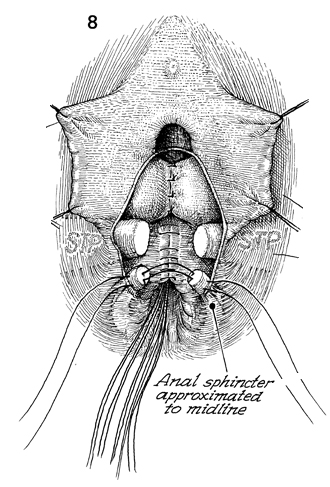
The levator plication has taken place over
the rectal suture line. The stumps of the superficial transverse
peritonea muscle must be identified, especially with their fascia
sheaths. The anal sphincter muscle should be identified, and
care should be taken to identify its fascia sheath. Sutures are
placed through the fascia sheath and muscle. Generally, four
sutures are used in a points-of-the-compass pattern. |
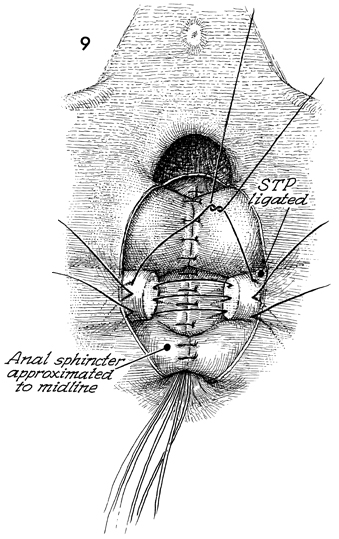
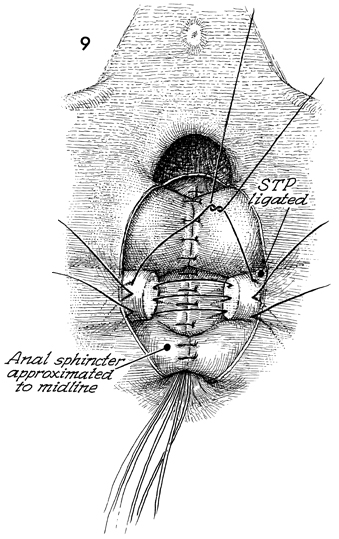
Figure 9 shows the rectal mucosa sutured.
The levator ani muscles have been plicated over the rectal mucosa,
the anal sphincter is plicated in the midline, and now the stumps
of the superficial transverse peritonea (STP) muscle
are identified, and sutures are placed in the fascia of this
muscle in a points-of-the-compass pattern. |
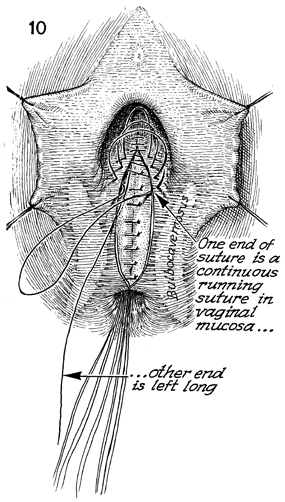
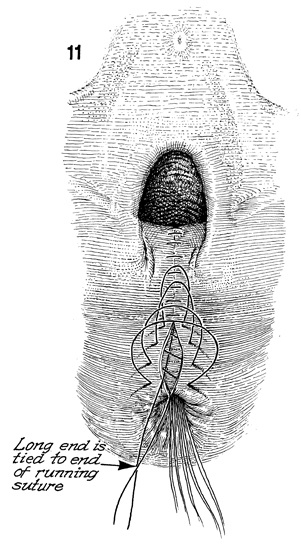
The vaginal mucosa is closed with a running
synthetic absorbable suture. Note that the knot is tied at the
top of the vagina, and one strand of the knot is left long, coming
on top of the levator repair underneath the vaginal mucosa. This
strand of suture, when tied, will further plicate the top of
the vagina posteriorly on top of the rectum, creating the so-called
hockey-stick pattern of the vaginal canal. |
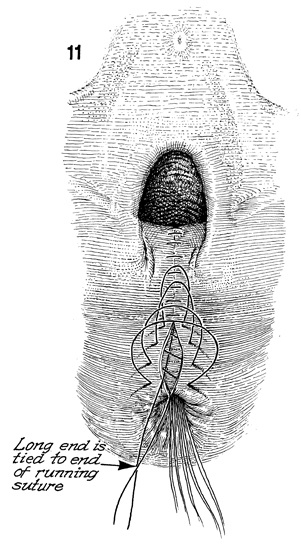
The suture has been extended
out over to the skin of the peritoneal body. Note that the long
end is tied to the end of the running suture. When this is performed,
the upper vagina is pulled posteriorly onto the rectum. |
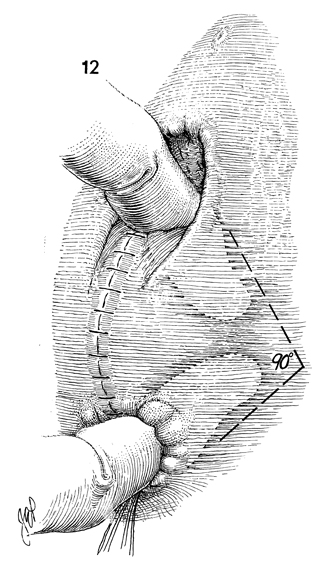
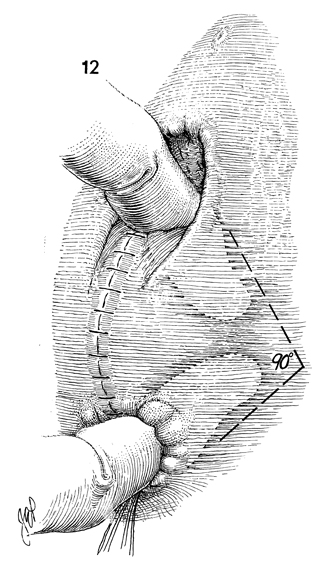
A finger could be inserted in
the vagina, and a finger should be inserted in the rectum. These
fingers should make a 90 dgree angle. Postoperatively, the patient
is placed on running daily doses of mineral oil and a low-residue
diet. We would prefer the patient have loose watery stools every
day for 2 weeks. After each watery stool, she should be cleaned
with a septic solution. |
|