Vagina
and Urethra
Anterior Repair and Kelly
Plication
Site Specific Posterior Repair
Sacrospinous
Ligament Suspension of the Vagina
Vaginal Repair of Enterocele
Vaginal Evisceration
Excision of
Transverse Vaginal Septum
Correction of
Double-Barreled Vagina
Incision
and Drainage of Pelvic Abscess via the Vaginal Route
Sacral Colpoplexy
Le Fort Operation
Vesicovaginal Fistula
Repair
Transposition
of Island Skin Flap for Repair of Vesicovaginal Fistula
McIndoe Vaginoplasty
for Neovagina
Rectovaginal Fistula
Repair
Reconstruction of
the Urethra
Marsupialization
of a Suburethral Diverticulum by the Spence Operation
Suburethral
Diverticulum via the Double-Breasted Closure Technique
Urethrovaginal
Fistula Repair via the Double-Breasted Closure Technique
Goebell-Stoeckel
Fascia Lata Sling Operation for Urinary Incontinence
Transection
of Goebell-Stoeckel Fascia Strap
Rectovaginal
Fistula Repair via Musset-Poitout-Noble Perineotomy
Sigmoid
Neovagina
Watkins Interposition Operation |
Sigmoid Neovagina
The use of intestine for a neovagina adds an additional procedure
to the formation of a neovagina. Traditional techniques for neovagina
have included myocutaneous flaps, skin grafts, skin grafts applied
to omental cylinders, and combinations thereof. The normal nonirradiated
sigmoid colon may represent an ideal structure to become a neovagina.
Unlike the small intestine, which has excessive necrotizing secretions,
the mucosa of the sigmoid colon has secretions that are less necrotizing
and less copious. The advantages of the sigmoid neovagina over skin
grafts of various kinds are (1) it has its own inherent blood supply
through the superior hemorrhoidal artery and sigmoid branches of that
artery; and (2) it has distensibility through compliance unavailable
in skin grafts. Although blood supply can be a positive aspect of sigmoid
neovagina, the blood supply is critical. If for some reason the inferior
mesenteric artery or the superior hemorrhoidal branch of the inferior
mesenteric artery is compromised, the blood supply to the neovagina
will be lost. A negative feature of sigmoid neovagina is that it requires
an intestinal anastomosis between the descending left colon and the
remaining rectum.
Points of Caution. Adequate
mobilization of the descending colon must be achieved to prevent
tension on the anastomosis. Adequate visualization of the superior
hemorrhoidal artery and its sigmoid branches must be obtained.
The
use of the vaginal form is controversial. There are those who believe
that packing or a vaginal form is not necessary. Other surgeons routinely
use foam rubber covered with a condom as a vaginal form to maintain
dilation of the colon and/or neovagina.
Technique
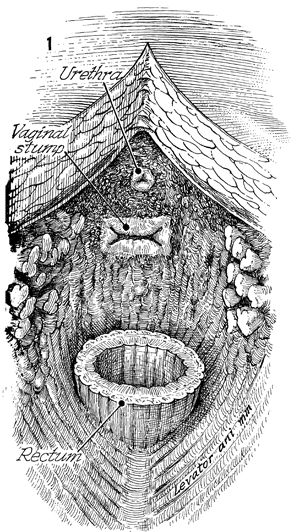
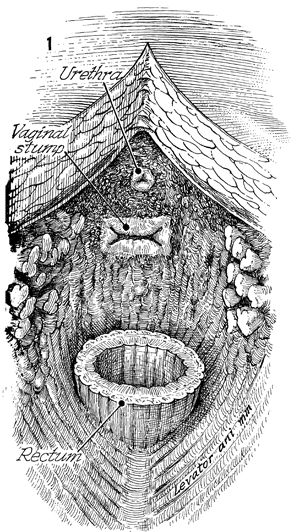
Figure 1 shows a view of the pelvis
in which a total supralevator exenteration has been performed.
The stump of the urethral meatus, the stump of the vagina at
the level of the introitus, and the stump of the rectum at the
level of the peritoneum are noted. |
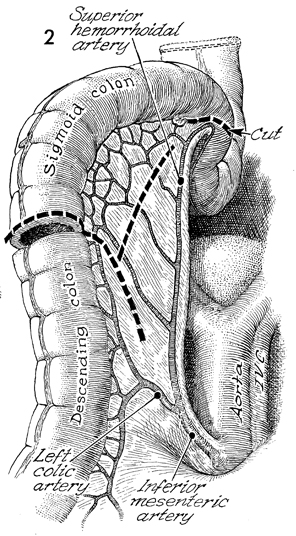
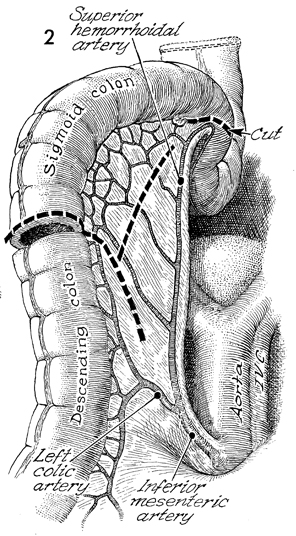
Sigmoid neovagina is begun by mobilizing
the left colon including the splenic flexure of the transverse
colon. The inferior mesenteric artery and its branches, the left
colic artery and the superior hemorrhoidal artery, are carefully
identified. A segment of sigmoid colon approximately 14 cm long
is selected. The colon is transected, the marginal artery of
the colon is divided, and the incision is extended along the dotted
line into the mesentery. At this point, several branches
of the superior hemorrhoidal artery that feed the sigmoid branches
are identified. An incision is made in the mesentery to the sigmoid
colon neovagina, leaving several branches of the superior hemorrhoidal
artery intact to act as blood supply for the entire colonic segment
neovagina via the margin artery of the colon. IVC indicates
the inferior vena cava. |
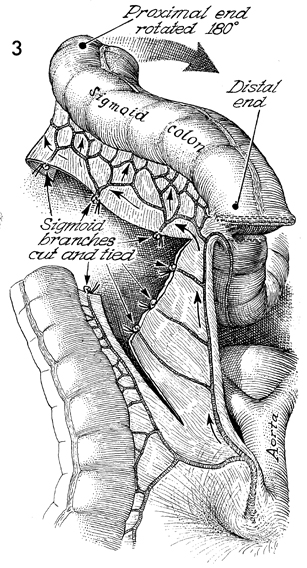
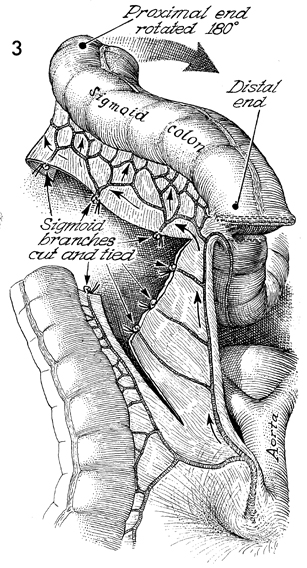
The transection into the mesentery
and parallel to the colon within the mesentery but beneath the
network of marginal vessels to the colon is necessary for the
segment to be rotated into the antiperistaltic position to reach
the vaginal introitus. That is, the proximal end of the sigmoid
neovagina is rotated 180°, and the distal end of the colon
now becomes the proximal end of the neovagina. This 180° rotation prevents excessive tension on the superior hemorrhoidal
artery, jeopardizing its integrity. |
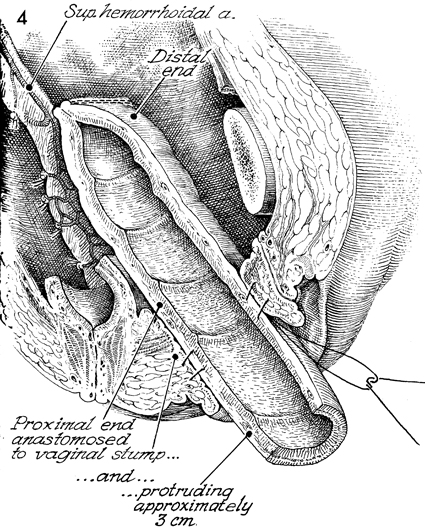
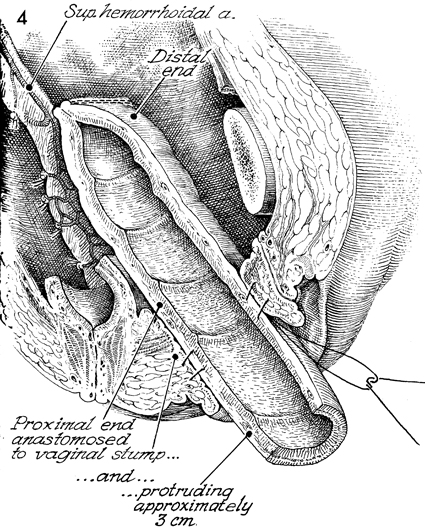
The proximal end of the sigmoid
colon is pulled through the vaginal introitus. A prolapse of
colon protruding approximately 3 cm out of the introitus is created,
and sutures are placed between the colonic wall and introitus.
A 3-4 cm segment of prolapse is essential because in the immediate
postoperative period there will be tendency for retraction. If
the surgeon transects the colon flush with the introitus, there
will be postoperative retraction and stricture. Note here that
the rectal stump is still in place for a very low end-to-end
anastomosis between the left colon and the rectum with the EEA
stapler, performed in the routine manner as seen in the section
Colon. |
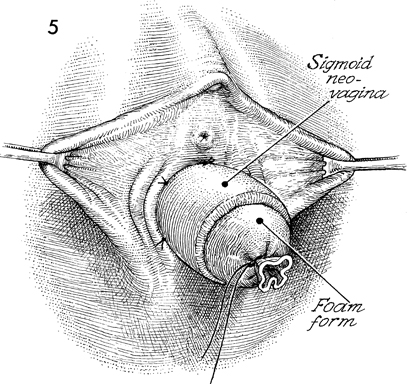
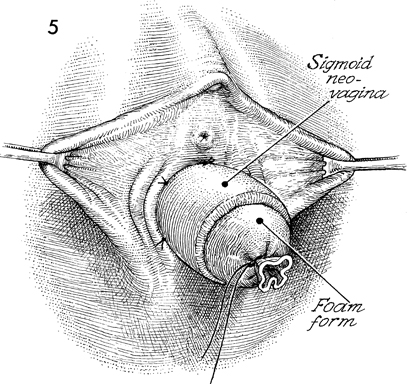
The completed operation shows
a soft foam rubber vaginal form in the sigmoid neovagina, which
is protruding 3-4 cm outside the introitus and is sutured into
place for a minimum of 2-3 weeks. Excess prolapsed colon can
be trimmed with an electric cautery as an out-patient procedure.
After the wounds have healed, we do not continue to use the neovaginal
foam rubber form. Sexual intercourse is allowed as soon as the
patient's wounds have healed and it becomes comfortable. |
|
|