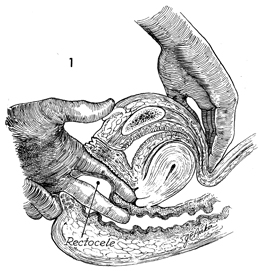
Posterior repair is performed in conjunction with perineorrhaphy to
correct a rectocele and to reconstruct the perineal body. A rectocele
is a hernia that develops when the perirectal fascia is insufficient
to support the anterior rectal wall and the rectum prolapses through
the levator sling. The strength of the posterior vaginal mucosa is
insufficient to prevent prolapse of the anterior rectal wall.
The purpose of posterior repair is to plicate the perirectal
fascia over the anterior rectal wall and provide a two-layer closure
of this hernia.
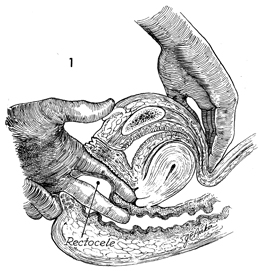
The patient is placed in the dorsal lithotomy
position. The pelvis and large intestine are prepared for surgery.
A bimanual examination under general anesthesia
is performed to differentiate between an enterocele and a rectocele.
Observation of the perineal body is made to determine the extent
of reconstruction needed. |

The labia are retracted with interrupted
sutures. The upper extent of the rectocele is identified. Allis
clamps are applied to the posterior vaginal mucosa over this
area. The clamps are elevated, creating a triangle. |
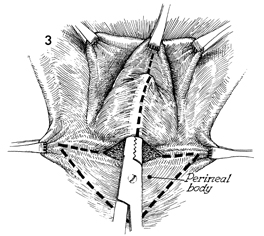
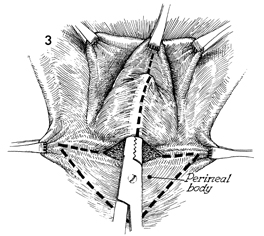
Allis clamps are placed at the margins
of the original hymen. An additional Allis clamp is placed
in the midline at the top of the rectocele. A transverse incision
is made at the posterior fourchette. A Kelly clamp is inserted
under the posterior vaginal mucosa, dissecting the posterior
mucosa off the perirectal fascia. An additional incision is
made in the perineal body, removing a triangular piece of skin,
outlined by the dotted line. This will expose the
insertion of the bulbocavernosus muscle. Only the skin of the
perineal body should be removed, and care should be taken not
to remove the underlying superficial transverse perineal muscles. |

The vertical incision in
the posterior vaginal mucosa has been made, and the edges are
held with Allis clamps. The perirectal fascia is dissected
off the posterior vaginal mucosa. The apex of the rectocele
is held in an Allis clamp. The dissection of perirectal fascia
off the vaginal mucosa is started with a scalpel but is completed
with the handle of the scalpel or with scissors. |
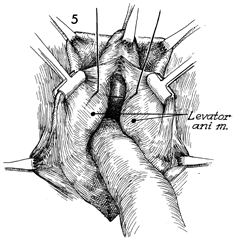
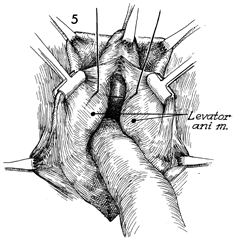
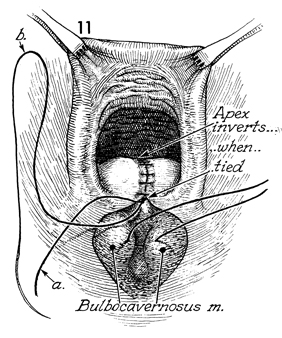
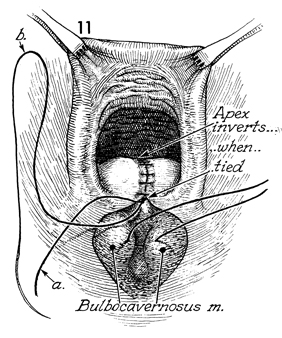
A finger is placed over the rectocele,
pushing it into the rectum, thus revealing the margins of the
levator ani muscles. A heavy, number 1 synthetic absorbable
suture is passed through the margin of the levator ani from
the apex down to the posterior fourchette. Frequently, 5-6
sutures are required to completely approximate the levator
ani. By depressing the anterior rectal wall downward with one
finger and elevating the previously placed suture, the surgeon
sees the margin of the levator ani more clearly, and placement
of sutures becomes easier. |
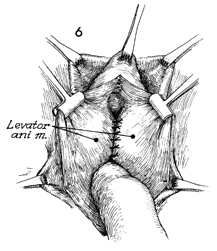
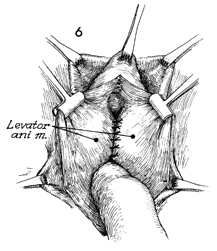
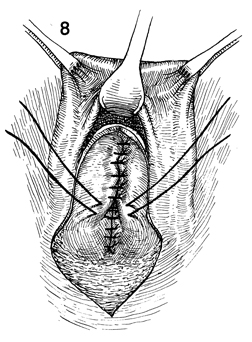
After all levator ani sutures
have been placed, they are progressively tied. |
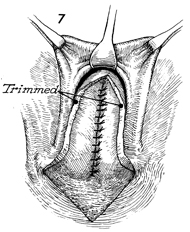
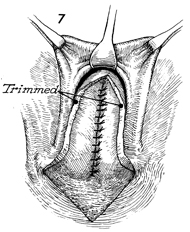
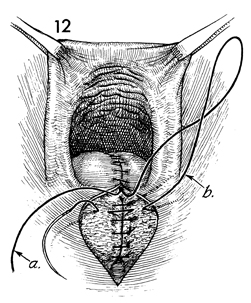
The excessive posterior vaginal mucosa has
been trimmed away; the triangular defect in the perineal body
can be seen. The insertion of the bulbocavernosus muscle is adjacent
to the triangular defect in the perineal body. |
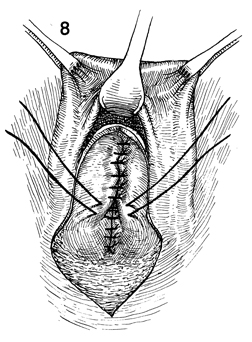
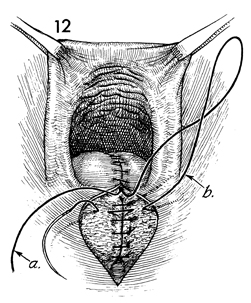
The perirectal fascia is closed with interrupted
0 synthetic absorbable suture in the midline |
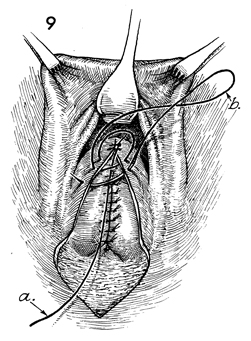
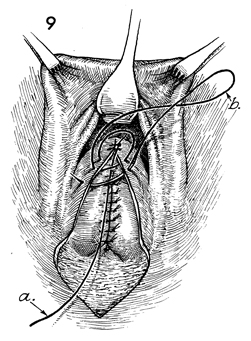
A 0 synthetic absorable suture is placed
at the apex of the vaginal mucosa and tied (a). The
tail of the suture is left for a length of 20 cm. The suture (b) is
placed superficial to the tail of the suture (a). |
The closure of the posterior vaginal wall
is completed to the posterior fourchette. The former hymenal
ring is reconstructed. The suture (b) is tied to the
tail of the first suture (a) placed at the apex. The
vaginal mucosa is approximated to the perirectal fascia to eliminate
dead space. |
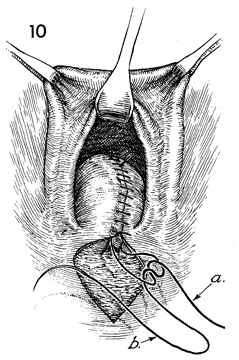
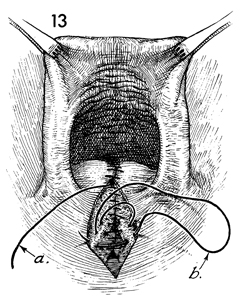
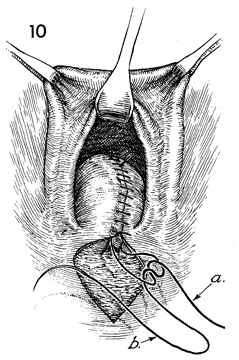
The same suture completes the closure of
the perineal body. Several interrupted 0 synthetic absorbable
sutures are placed in the insertions of the bulbocavernosus muscles
to reconstruct the perineal body. |
The posterior vaginal mucosa suture (b) is
placed in the subcutaneous tissue of the perineal body. Note
that the suture marked a is still left long for eventual
tying. |
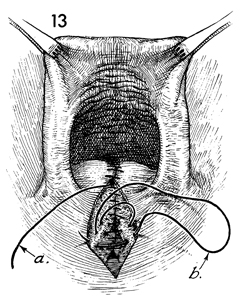
The same suture (b) that completed
the closure of the posterior vaginal wall is used to close the
subcutaneous tissue and the insertions of the bulbocavernosus
muscles. The suture marked a is the long end of the
tie at the apex of the posterior vaginal mucosa incision. |

The subcuticular suture (b) is placed
in the skin of the perineal body from the apex of the wound immediately
above the anus to the posterior fourchette. At the posterior
fourchette it is tied to suture a. |
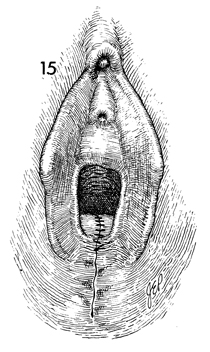
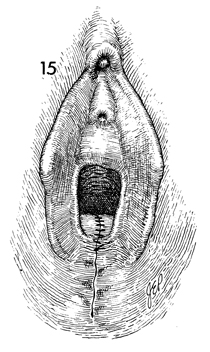
The completed operation is shown, with the
rectocele reduced and the perineal body reconstructed. Vaginal
packs are not required. Bladder catheterization is rarely indicated. |
|