|
||||||||
Anterior Repair and Kelly
Plication |
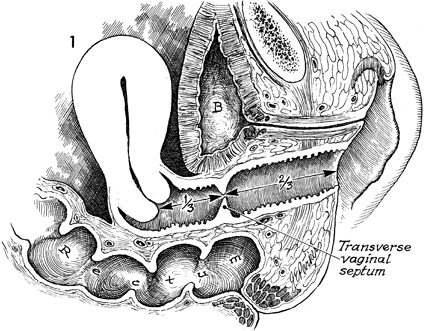
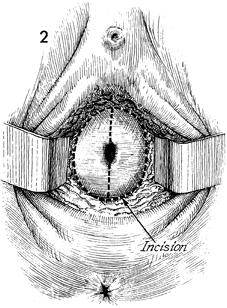
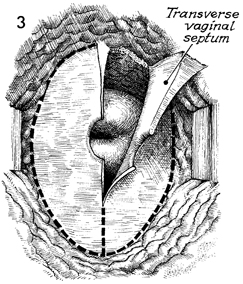
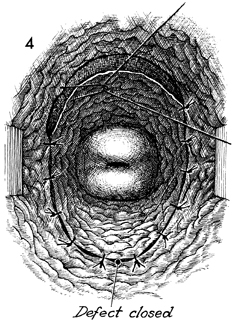
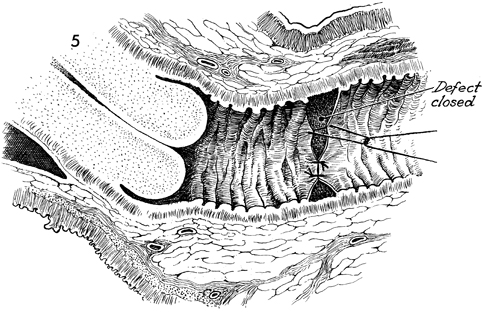
Excision of Transverse Vaginal Septum Transverse vaginal septum generally occurs between the upper one-third and lower two-thirds of the vaginal canal. This is additional evidence that the upper one-third of the vagina is of Mullerian origin and that the lower two-thirds of the vagina is embryologically developed via the urogenital sinus. The septum can be either complete or partial. If it is complete, the symptoms of vaginal obstruction occur at the time of menarche, since menstrual blood is entrapped above the septum and has no egress from the vagina. If the septum is partial, it may be discovered on a routine gynecologic examination, or the patient may present with dyspareunia. The operation is performed to remove the transverse vaginal septum without significantly shortening the vaginal canal. Physiologic Changes. The physiologic changes desired are (1) the egress of menstrual blood from the vaginal canal without obstruction and (2) the normal functioning of the vagina. Points of Caution. If the septum is complete and hematometra or hematocolpos is present, it is unwise to attempt surgical correction of the septum at the time the obstruction is relieved. The procedure of choice is incision and drainage of the hematometra or hematocolpos, with reconstruction delayed 6-8 weeks until the tissues have completely healed. To avoid unduly shortening the vagina, excessive vaginal mucosa should not be removed. Technique
|
|||||||
Copyright - all rights reserved / Clifford R. Wheeless,
Jr., M.D. and Marcella L. Roenneburg, M.D.
All contents of this web site are copywrite protected.