Bladder
and Ureter
Insertion
of Suprapubic Catheter
Retropubic
Urethropexy:
Marshall-Marchetti-Krantz
and Burch Operations
Ureteroureterostomy
Ureteroneocystostomy
and Ureteroneocystostomy
With Bladder Flap
Transperitoneal
Ureteroureterostom
End-to-Side Anastomosis
Intestinal
Loop
Urinary Diversion
Percutaneous
Nephropyelostomy
Ureteroileoneocystostomy
Clam
Gastrocystoplasty |
Percutaneous Nephropyelostomy
A suture ligature, excessive radiation, scarring from
radical surgery, or clamping the ureter all lead to hydroureter and
eventual hydronephrosis and loss of the kidney. If the ureter is transected,
urinary ascites will result and eventually lead to infection and abscess.
The
incidence of injury to the ureter associated with pelvic disease and/or
surgery ranges from 0.3% to 5%.
Injury to the ureter is a medical emergency. Time is of importance,
since for every hour that the kidney is obstructed, there is further
damage to the renal collecting system.
A straightforward and simple
procedure has been developed that avoids major surgery and relieves
the sequelae of ureteral injury and obstruction in most cases-percutaneous
needle nephropyelostomy.
Physiologic Changes. Percutaneous
nephropyelostomy relieves the obstruction and prevents death of the
renal nephron unit while corrective surgery can be planned.
Points of Caution. Fluoroscopy and ultrasound are
used to guide the needle through the cortex of the kidney into the
renal pelvis. Once the needle is in the renal pelvis, the guidewire
should be advanced down into the urinary tract as far as the bladder
if possible.
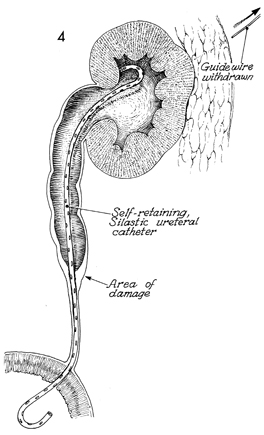
An attempt should be made to totally implant the "J"
or pigtail stent. Not having a catheter through the renal parenchyma
will reduce repeated episodes of gross hematuria. In some cases, however,
this cannot be done, and the stent must be brought out through the
renal cortex, flank wall, and skin and connected to a drainage bag.
Technique
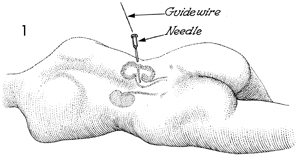
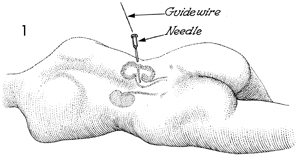
The patient is placed in the prone position
and rolled into the modified lateral decubitus position with
the hip and the knee flexed. The side representing the normal
kidney should be down, with the hip and the knee on that side
extended. Dye for an intravenous pyelogram has been injected.
The hydronephrosis is seen in the right kidney. |
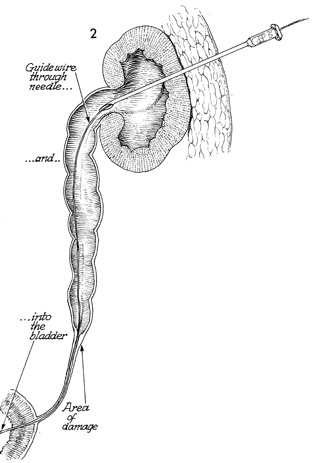
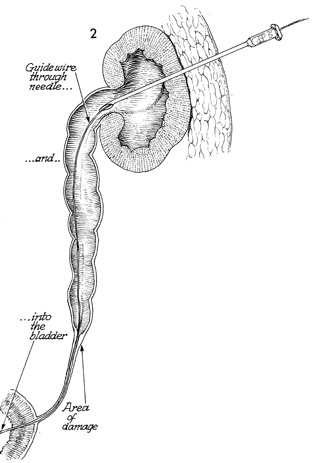
Under fluoroscopic control, the 16-gauge
Tuohy-type needle should be advanced through the abdominal wall
in the costovertebral angle area. The renal cortex should be
perforated, and the needle should be advanced into the renal
pelvis. Injection of a small amount of x-ray dye will confirm
that the needle is in the renal pelvis. At this point, a flexible
guidewire is threaded through the needle, down the ureter, under
fluoroscopic control. The area of damaged ureter is approached,
and if possible, the guidewire is manipulated through this area
of damage into the bladder. If this is not possible, the guidewire
should be threaded as close as possible to the area of damage. |
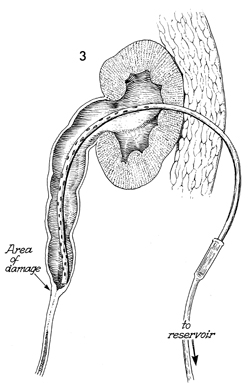
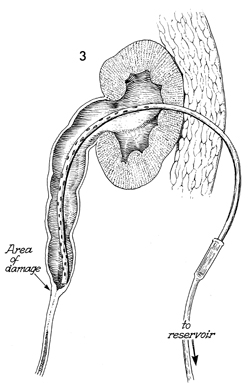
The needle is withdrawn, and
a double-J or pigtail catheter is inserted over the guidewire
through the flank wall, through the renal cortex, into the renal
pelvis, and down the ureter. Ideally, the double-J catheter
should be inserted through the area of ureteral damage into the
bladder. Injection of small amounts of contrast medium can confirm
its position. |
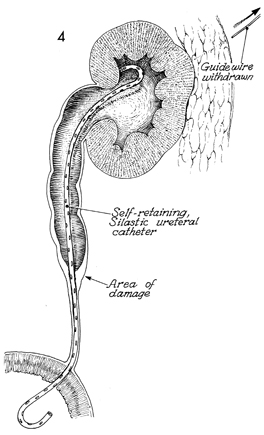
By using a tubular pusher over the guidewire,
the surgeon can advance the proximal end of the "J" catheter
through the flank wall and the renal cortex into the renal pelvis.
This leaves the proximal end of the catheter stent in the renal
pelvis and the other end in the bladder. |
|