Bladder
and Ureter
Insertion
of Suprapubic Catheter
Retropubic
Urethropexy:
Marshall-Marchetti-Krantz
and Burch Operations
Ureteroureterostomy
Ureteroneocystostomy
and Ureteroneocystostomy
With Bladder Flap
Transperitoneal
Ureteroureterostom
End-to-Side Anastomosis
Intestinal
Loop
Urinary Diversion
Percutaneous
Nephropyelostomy
Ureteroileoneocystostomy
Clam
Gastrocystoplasty |
"Clam"
Gastrocystoplasty
Pelvic radiation is frequently necessary for the treatment
of gynecologic cancer. Normally, the bladder tolerates irradiation
therapy up to 7000 cGy without significant sequela. In some patients,
however, radiation fibrosis develops, creating a small stiff bladder
with low capacity and high pressure resulting in total incontinence
of urine. Frequently, these patients have a low urethral pressure but
an extremely high vesical pressure. The usual urogynecologic pin-up
surgical procedures, e.g., the Marshall-Marchetti-Krantz or Burch operations
will not alter the physiologic changes that created the problem, i.e.,
radiation fibrosis of the bladder.
A source of nonirradiated highly
vascular tissue placed in the wall of the bladder for augmentation
can relieve this disabling and incapacitating situation.
There are cases
in which the patient has received no radiation but has a severe detrusor
instability of the bladder with total incontinence. Transecting the
bladder in the longitudinal plane produces some denervation of the
bladder and reduction of detrusor instability. The augmentation of
stomach to the transected bladder is referred to as a "clam" procedure
and can relieve the incontinence.
Physiologic Changes. The physiologic
sequela of removing a small gastric flap from the grater curvature
of the stomach has few if any consequences. The augmentation of an
opened bladder with this gastric flap has significant physiologic changes.
The bladder capacity increases significantly. The usual bladder capacity
of a radiation-fibrosed bladder is less than 100 mL. The gastric flap
increases the bladder capacity from 300 to 500 mL.
The gastric flap
secretes acid. This gives the patient an acid urine that creates an
unfavorable environment for bacterial growth.
The gastric flap is quite
distensible. Because of this distensibility the bladder, when full
of urine, will have a low pressure, usually in the range of 30-40 cm
of water. If the urethral pressure has a natural pressure of 70-80
cm of water, continence will be restored. If the urethral pressure
is low, continence will be improved if a Goebell-Stoeckel fascia lata
sling operation in addition to the clam gastrocystoplasty is performed
(see Vagina and Urethra), for discussion of the Goebell-Stoeckel fascia
lata sling.
Technique
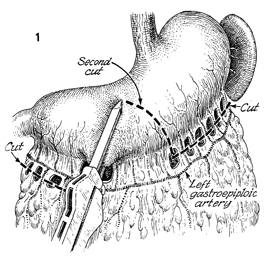
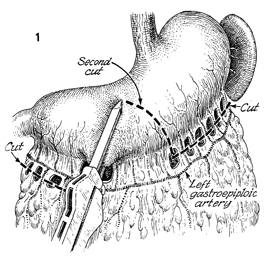
Figure 1 shows the esophagus, stomach, spleen,
and omentum. The left gastroepiploic artery for this flap is
shown, although the right gastroepiploic artery works equally
well. The defects in the mesentery between the short gastric
arteries are made, and each short gastric artery is cut and tied.
The right gastroepiploic artery is transected at the junction
of the duodenum and each of the branches of the right gastroepiploic
artery and transected and tied. The GIA (gastrointestinal anastomosis)
stapler is placed across the stomach for approximately 6 cm.
The base of this triangular flap will be approximately 6 cm. |
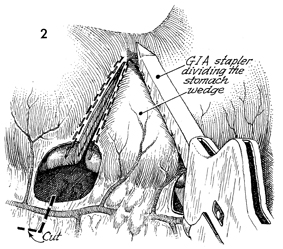
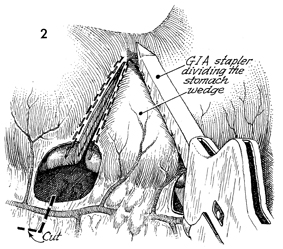
The right gastroepiploic artery has been
transected (bottom). The right side of the wedge of
stomach has been cut and stapled. The left portion of the wedge
flap is shown with the GIA stapler dividing both the anterior
and the posterior gastric wall. |
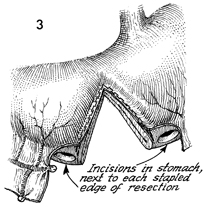
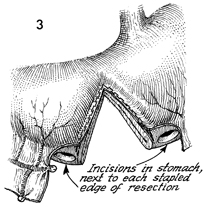
The defect in the stomach is shown, and small
incisions are made for a gastrotomy in the proximal and the distal
stomach. |
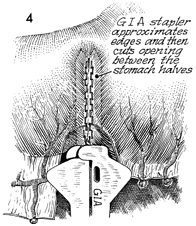
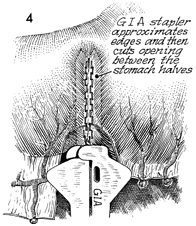
A GIA stapler is placed in the small gastrotomy
incisions on the greater curvature. The GIA stapler reapproximates
the stomach and then cuts between the edges to reestablish continuity. |
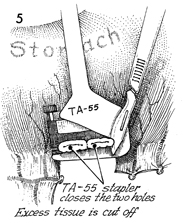
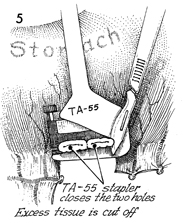
The remaining defects created by the small
stab wound gastrotomies are picked up with Babcock clamps and
cross-clamped and stapled with a TA-55 4.8 stapler. The TA-55
stapler closes the two gastrostomy defects. Excessive tissue
is cut away. |
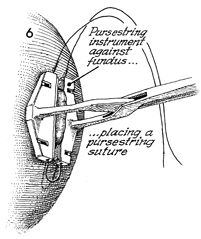
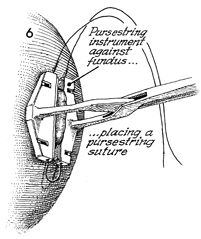
A feeding tube gastrostomy
is placed in the stomach for decompression and possible total
enteral nutrition if needed. The procedure is initiated by placing
the automatic pursestring suture device across the stomach wall
8-10 cm proximal to the resected and reconstituted gastric flap. |
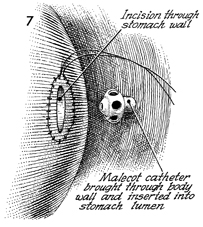
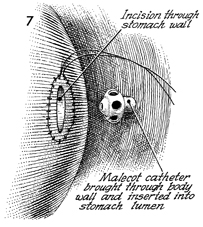
A small gastrotomy is made in the center
of the pursestring suture. A stab wound is made in the left upper
quadrant of the abdomen, and a No. 22 French Malecot catheter
is brought through the abdominal wall to be inserted into the
lumen of the stomach. |
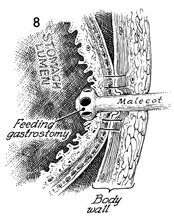
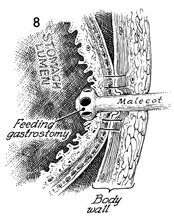
Figure 8 shows the stomach
lumen, the abdominal wall, and the feeding tube gastrostomy catheter
(Malecot) in place. The visceral peritoneum of the stomach is
sutured to the parietal peritoneum to prevent leakage of gastric
juice until mesothelialization has sealed the wound. |
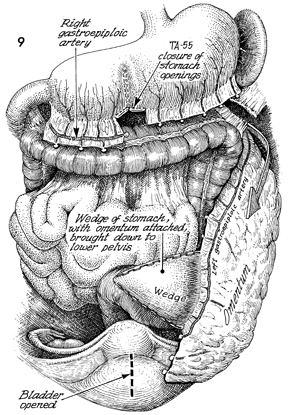
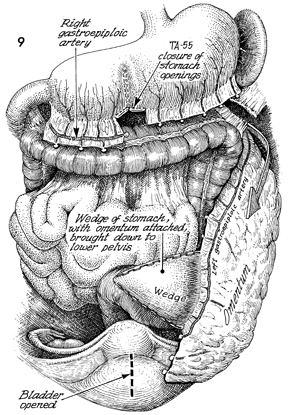
The right gastroepiploic artery on the greater
curvature of the stomach, a branch of the celiac artery, is shown
transected and tied. The remaining short gastric branches of
the left gastroepiploic artery are seen transected and tied.
The omentum with its attached gastric flap is shown lateral to
the left colon. It is placed in the left descending colonic gutter
along the line of Toldt. The wedge of stomach with omentum attached
is brought down into the lower pelvis. In the bottom portion
of this figure, the incision line into the bladder is shown,
thus creating an opening shaped like a sea clam. This linear
incision (broken line) in the bladder offers a wide
defect. Those patients with severe detrusor instability have
reduced, uncontrolled contractions of their bladder. |
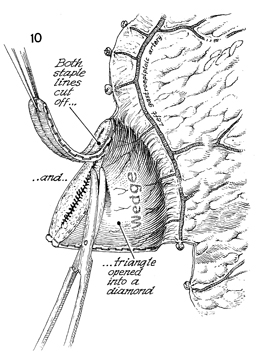
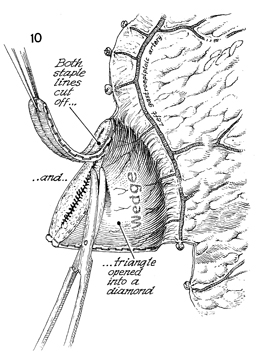
Figure 10 shows the left gastoepiploic artery
with its short gastric branches feeding the wedge of the gastric
flap. All staples must be completely removed. The presence of
staples will create stones in the bladder. The triangle gastric
flap is open and now forms the shape of a diamond. |
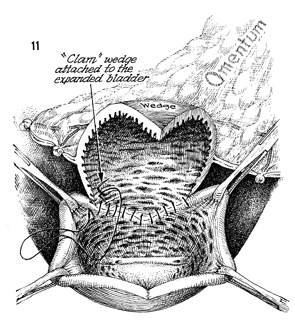
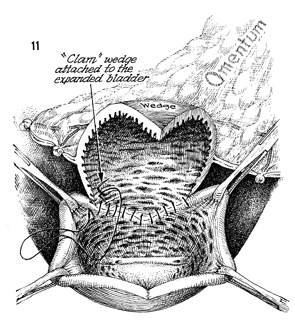
The longitudinally opened bladder is shown-thus
its description as a clam. The gastric diamond-shaped flap is
sutured into the bladder defect. The suture material should be
synthetic absorbable.
|
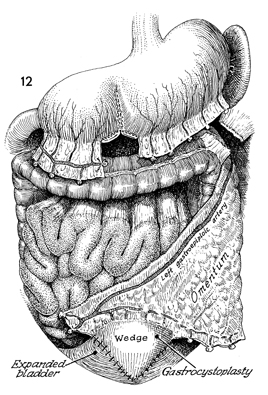
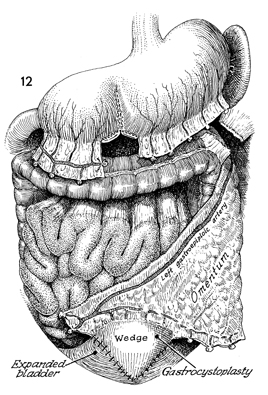
At the bottom, the diamond-shaped wedge of
stomach is seen sutured in place to the clam gastrocystoplasty-opened
bladder, while the reconstituted stomach with its staple line
is shown at the top.
We frequently place two Foley
catheters in the reconstructed bladder. A transurethral No. 16
French Foley catheter with a 5-mL bag is placed through the urethra
into the reconstructed bladder. We frequently perform a small
cystotomy 3 cm away from the gastric wedge suture line to insert
a second Foley catheter as a suprapubic cystotomy. This double
drainage guards against the possibility of mucus produced by
the gastric artery plugging up one of the Foley catheters, thus
allowing the possibility of a disrupted suture line through elevated
hydraulic pressure. A Jackson-Pratt suction drain is brought
through the anterior abdominal wall and placed near the bladder
suture line. The Foley catheter is left in the bladder for approximately
2 weeks. When drainage has ceased, the Jackson-Pratt suction
drain is removed. The patient initiates timed voiding by bearing
down. The patient should void every 4-6 hours. Patients are discouraged
from getting up at night to void; they are encouraged to void
immediate upon arising.
All feedings are initiated when
there are excellent bowel sounds and a bowel movement. At this
time it will be safe to remove the tube gastrostomy. |
|