Fallopian Tubes
and Ovaries
Laparoscopy
Technique
Diagnostic
Uses
of Laparoscopy
Demonstration
of Tubal Patency
via Laparoscopy
Laparoscopic
Resection
of Unruptured
Ectopic Pregnancy
Ovarian
Biopsy
via Laparoscopy
Electrocoagulation
of
Endometriosis via
Laparoscopy
Lysis
or Adhesions
via Laparoscopy
Control
of Hemorrhage
During Laparoscopy
Fallopian
Tube
Sterilization
Sterilization
by
Electrocoagulation and
Division via Laparoscopy
Silastic
Band Sterilization
via Laparoscopy
Hulka
Clip Sterilization
via Laparoscopy
Sterilization
by the
Pomeroy Operation
Sterilization
by the
Modified Irving Technique
Sterilization by the
Minilaparotomy Technique
Sterilization - Ucheda Technique
Salpingectomy
Salpingo-oophorectomy
Fimbrioplasy
Tuboplasty
-
Microresection
and Anastomosis
of the Fallopian Tube
Wedge
Resection
of the Ovary
Torsion
of the Ovary
Ovarian
Cystectomy |
Laparoscopy Technique
The basic procedures for laparoscopy are the same whether
this form of surgery is used for diagnosis or surgical treatment. Either
a single- or a multi-incision technique may be employed. For the former,
the operative laparoscope is used. For the latter, the laparoscope
without operative channels is passed through the first incision, and
one or more operative instruments are inserted through the other incision
as required. The operative scope is attached to a video monitor to
enlarge the operative field and allow the operating room team to observe
the procedure. In simple diagnostic or surgical procedures, the operative
laparoscope has an advantage over the diagnostic laparoscope in that
it allows an operative instrument to be passed down its channel either
to stabilize structures or to aspirate blood or fluid from the operative
field.
The operation is a simple, safe, cost-efficient way
of diagnosing and treating problems within the female pelvis.
Physiologic Changes. Physiologic
changes occur when laparoscopy is used to lyse adhesions, fulgurate
endometrial implants, biopsy ovaries, remove ectopic pregnancies,
and relieve obstruction in the Fallopian tube or obstruct the tube
for sterilization by electrocauterization and/or the application
of a Silastic ring or clip.
Points of Caution. Care must be taken to ensure that
the needle for pneumoperitoneum is within the peritoneal cavity. The
trocar should always be kept sharp, or a disposable tocar should be
used. Electrocauterization should proceed with extreme caution.
Technique
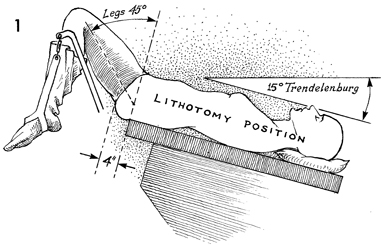
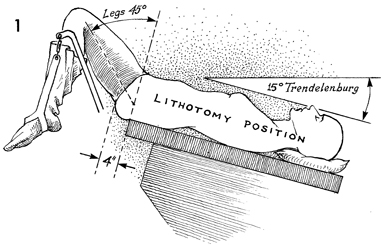
The surgeon who is knowledgeable
about all aspects of laparoscopy should position the patient
in the lithotomy position modified to conform to the special
requirements of the procedure. The legs are not placed in the
standard 90° flexion, as in
the classic dorsal lithotomy position, but are positioned at
45°flexion
from the hip. It is extremely important to have the buttocks
at least 4 inches off the end of the operating table to facilitate
manipulation of the cervical and intrauterine instruments into
an advantageous position for maximum visualization of the internal
genitalia. The operating table should be slanted to a 15° Trendelenburg
position to displace the intestines out of the pelvis and into
the upper abdomen. It is more comfortable for the operating surgeon
to have the patient's arms down at her sides than extended on
an arm board. We frequently insert the needle for intravenous
infusion into the forearm, then place the arm at the patient's
side and secure it with a draw sheet that has been previously
placed underneath the patient. |
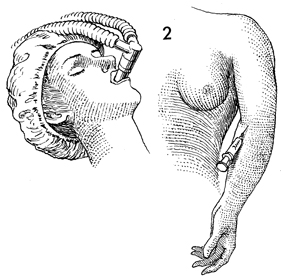
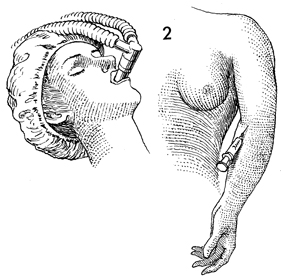
Anesthesia for laparoscopy can be either
general or local. If general anesthesia is used, it should be
administered by the same standard techniques as used for major
abdominal operations. One should not attempt to achieve surgical
planes of anesthesia with tranquilizers or narcotics.
If local anesthesia is used,
it should be accompanied by intravenous sedation prior to the
operative procedure. We prefer to sedate the patient with 50
mg meperidine (Demerol) and 10 mg diazepam (Valium) after she
is placed on the operating table. In general, we limit our use
of local anesthesia to laparoscopy sterilization procedures and
other short diagnostic procedures that do not require extensive
intraperitoneal manipulation of the tubes or ovaries. |
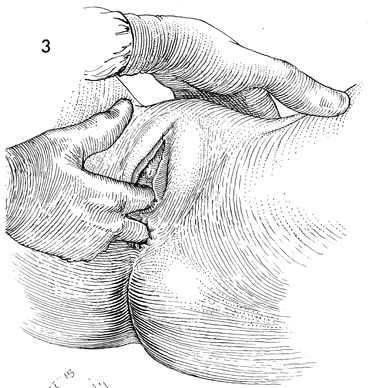
A bimanual pelvic examination should precede
all laparoscopy procedures. |
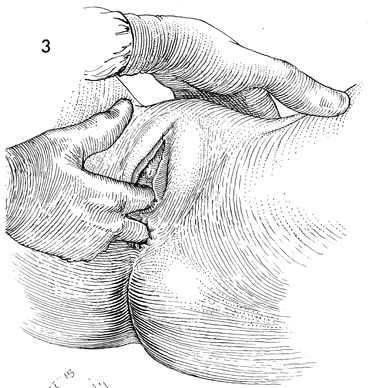
The procedure is started by
grasping the anterior lip of the cervix with a wide-mouthed Jacobs
tenaculum attached to a Rubin intrauterine cannula. Exposure
of the cervix should be obtained with a narrow curved Sims posterior
retractor rather than a wide, flat, posterior vaginal retractor.
The large retractors produce pain, sometimes initiating a cycle
of pain and anxiety that may make local anesthesia ineffective. |
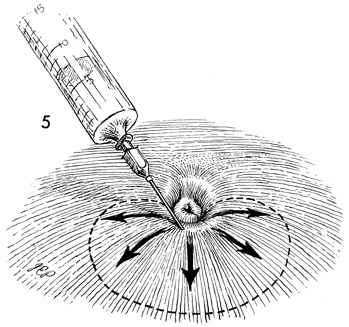
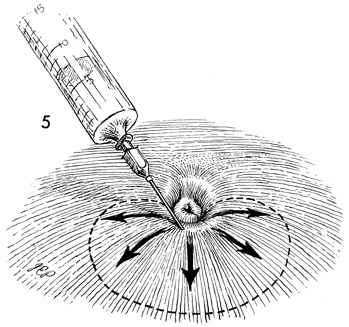
If local anesthesia is used,
the inferior rim of the umbilicus is thoroughly infiltrated with
1% Xylocaine solution in a semicircular manner from the 9 o'clock
position around to the 3 o'clock position on the umbilicus. The
first injection of Xylocaine should be given at the 6 o'clock
position on the inferior rim of the umbilicus, and the needle
should be advanced underneath the skin as shown. In addition,
approximately 2 mL should be infiltrated into the rectus fascia
and muscles. |
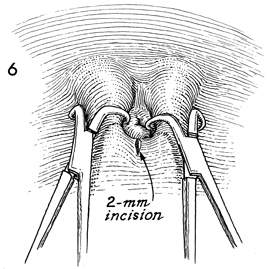
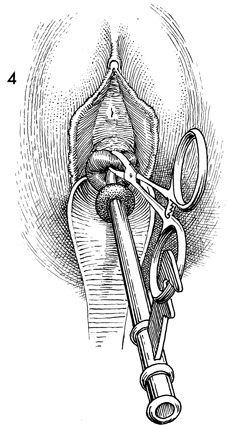
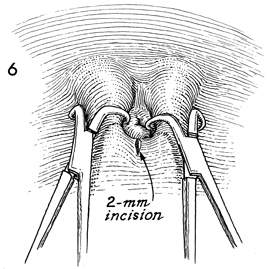
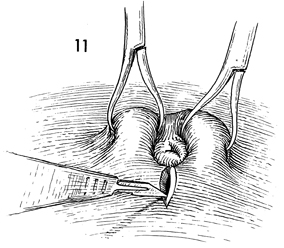
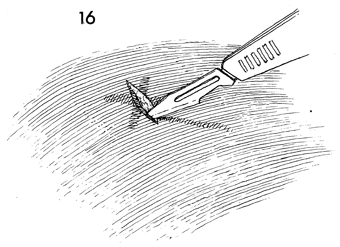
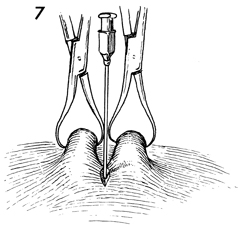
Adequate
countertraction on the anterior abdominal wall is necessary.
Although some rely on a large pneuoperitoneum to provide adequate
countertraction, we elevate the lower midline of the abdomen
for this purpose. We have found that placement of the two towel
clips, one each at the 5 and 7 o'clock positions on the inferior
rim of the umbilicus, offers the best method of countertraction
for insertion of the pneumoperitoneum needle and the trocar.
After the towel clips have been placed, a 2-mm incision is made
in the inferior rim of the umbilicus. |
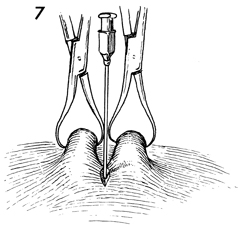
The towel clips are elevated slightly and
a 17-gauge Tuohy epidural needle is advanced through the 2-mm
incision down the fascia. |
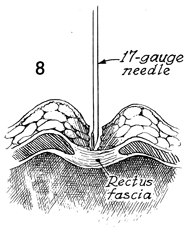
No attempt is made to penetrate the fascia
with the initial insertion of the Tuohy needle. |

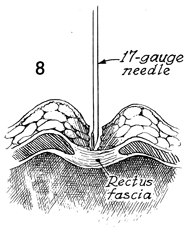
The needle is tapped against
the fascia several times at a 90° angle to the plane of
the body. The towel clips are further elevated for countertraction,
and the needle is pushed through the rectus fascia with a short
quick motion that advances the needle through the peritoneum.
This technique reduces the possibility that the needle will slide
off the rectus fascia and into the subcutaneous space. |
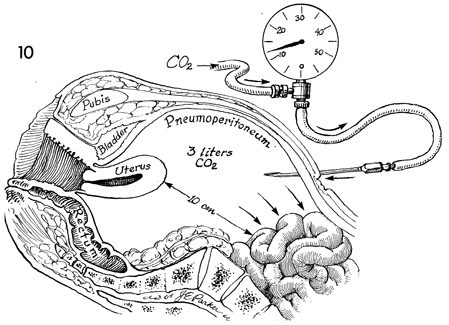
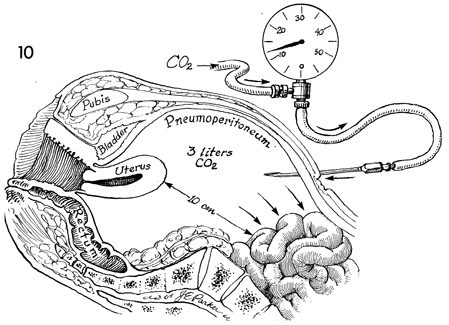
The pneumoperitoneum needle
is immediately attached to the gas line from the carbon dioxide
machine. The gas is allowed to flow and the pressure is observed
to ensure that it is approximately 15 mm Hg. We have found the
gas pressure method to be the most accurate way to determine
proper placement of the pneumoperitoneum needle. Other techniques
are the water-drop test and the saline-syringe test. With the
gas pressure method, using a large-bore 17-gauge needle, a pressure
greater than 15 mm Hg is an indication that the pneumoperitoneum
needle is not in the free peritoneal space but is either up against
a piece of bowel, in the omentum, or in the supraperitoneal space.
It should be further adjusted by advancing it, twisting the bore
180° or withdrawing it slightly until such time as the
pressure manometer indicates a pressure of less than 15 mm Hg.
There are times when the gas line or the needle itself has an
intrinsic obstruction that results in elevated false gas pressure
readings. In these cases, one would accept a gas pressure of
10 mm Hg above the baseline pressure. Generally, for sterilization
procedures such as the Silastic band operation, no more than
2 liters of carbon dioxide are needed. In electrocoagulation
of the Fallopian tubes or other surgical procedures, however,
a higher volume of gas is needed in order to obtain a larger
displacement of bowel away from the pelvic organs to reduce the
possibility of gastrointestinal burns. For diagnostic procedures,
it is better to use at least 4-5 liters of gas for maximum displacement
of bowel. Therefore, it is better to perform diagnostic and more
extensive surgical procedures under general anesthesia, as few
patients can tolerate 5 liters of gas in the peritoneal cavity
under local anesthesia. |
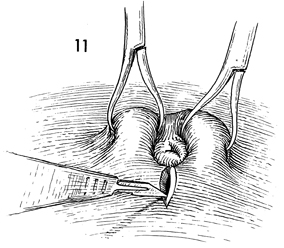
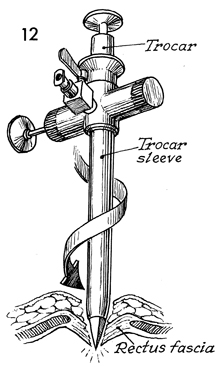
The 2-mm incision is extended to 1 cm. |
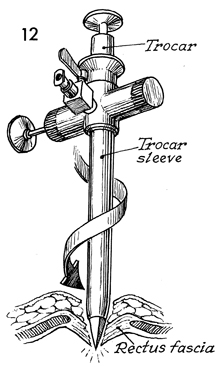
The laparoscope trocar and sleeve are inserted
through the umbilicus incision in a twisting corkscrew technique
that involves pushing the trocar down to the rectus fascia; with
a short twisting corkscrew motion, the trocar is pushed through
the rectus fascia while pulling up on the towel clips for countertraction.
By using the short thrust and corkscrew motions, the surgeon
advances the instrument progressively through the rectus fascia,
avoiding a sudden thrust that might slip and contact the intra-abdominal
or retroperitoneal organs. |
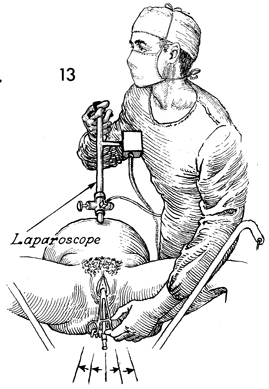
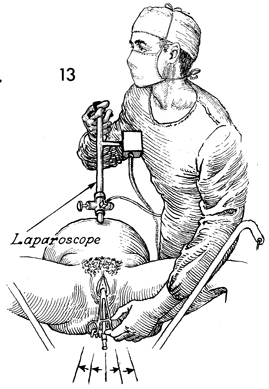
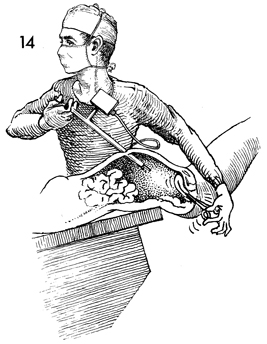
The trocar is removed from the
sleeve, the gas hose is connected to the gas port on the trocar,
and the laparoscope is advanced down the trocar sleeve into the
pelvis. The angle of the insertion of the laparoscope through
the sleeve and through the abdominal wall should be approximately
15-20° to the plane of the patient and not at 90° angle, to avoid touching the lens against the surface of the
bowel and the omentum. Such contact produces a pink or yellow
blur instead of the recognizable abdominal structures. By holding
the laparoscope in the right hand and moving the left hand between
the patient's legs and grasping the Jacobs tenaculum and Rubin
cannula, the uterus can be manipulated to either side or in the
anterior-posterior plane for maximum visualization of all the
internal genitalia. |
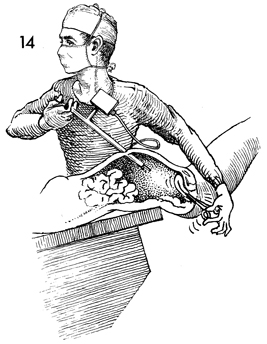
By depressing the Rubin cannula
and Jacobs tenaculum, the surgeon can move the uterus into an
anteflex position, thereby making the cul-de-sac, broad ligament,
tubes, and ovaries visible. When maximum visualization of the
structures is achieved, a nurse or assistant holds the Rubin
cannula and Jacobs tenaculum in the desired position while the
laparoscopist moves his left hand
up to support the operating laparoscope and his right hand to
perform the surgery (obviously, the reverse is true for those
surgeons who are left-handed).
|
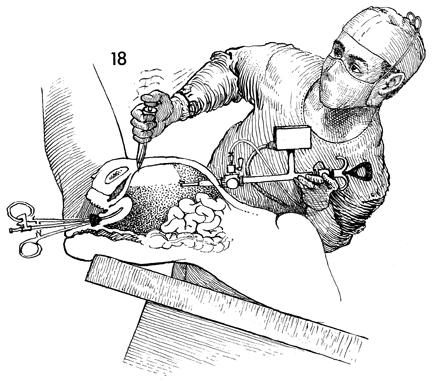
Multi-incision
Technique
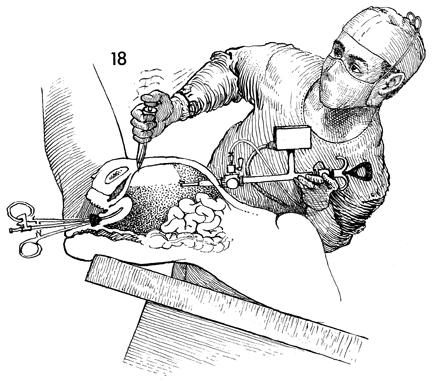
Multi-incision laparoscopy
is useful in most advanced surgical techniques. These cases
include egg retrieval for in vitro fertilization, ovarian biopsy,
extensive lysis of adhesions, extensive fulguration of endometriosis,
the occasional removal of an intraperitoneal foreign body,
laparoscopy-assisted vaginal hysterectomy, and resection of
ectopic pregnancy. |
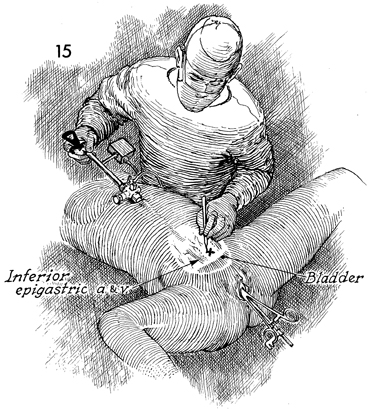
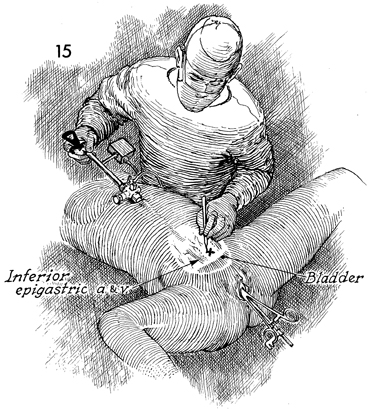
The first step in the insertion of a second
instrument is to transilluminate the lower abdominal wall and
select an avascular site for the incision of the second-incision
trocar. We prefer the left and right lower quadrants where it
is more advantageous to have the second-incision instrument at
a right angle to the first-incision observation instrument. In
all cases, however, an avascular area of the lower abdomen should
be selected with special care to avoid the inferior epigastric
artery and vein lateral to the rectus muscle. |
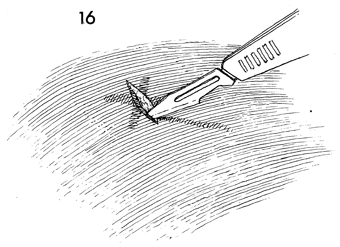
A 6-mm incision is made over the avascular
area down to the fascia, and the fascia is lightly incised with
the scalpel. |

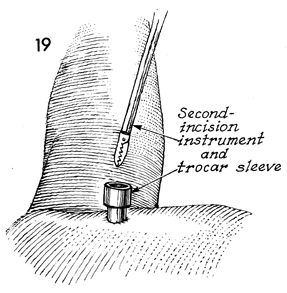
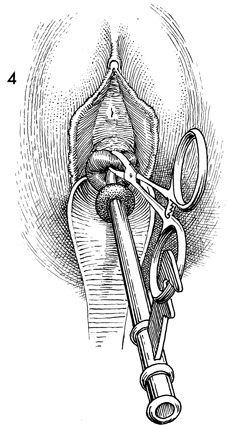
The second-incision trocar and sleeve are
held in a dagger fashion with the thumb on top of the trocar
and the fingers wrapped around the trocar sleeve. |
The second-incision trocar and
sleeve are inserted through the second-incision down to the fascia.
At this point, the surgeon looks through the laparoscope or the
attached video screen and slowly advances the second-incision
instrument until it has perforated the peritoneum. Occasionally,
it may be helpful to use the first-incision instrument as a source
of countertraction by using it to elevate the anterior abdominal
wall against the area where the second-incision trocar and sleeve
are penetrating the peritoneum. |
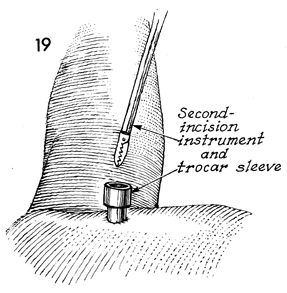
The second-incision trocar is withdrawn from
the second-incision sleeve and is now ready to receive operative
instruments. |
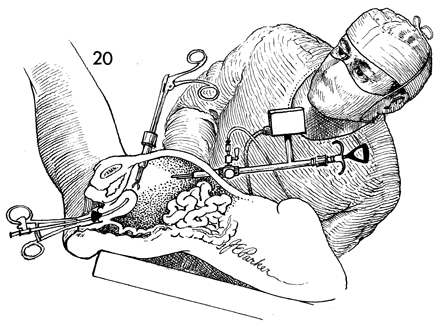
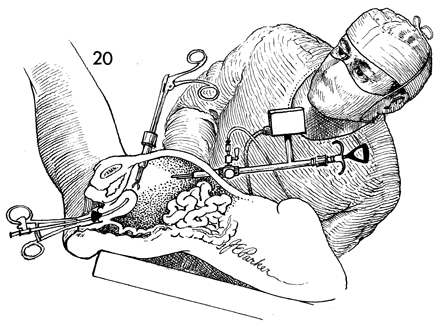
The Rubin cannula and Jacobs
tenaculum are held by a nurse or assistant in the most advantageous
position. The surgeon holds the laparoscope with his left hand
and the second-incision instrument with his right hand. Note,
that as shown, an operating laparoscope is used for the first
incision. This allows a second instrument to be inserted into
the abdominal cavity to facilitate the desired surgery without
a second incision. The ovary or Fallopian tube can be stabilized
for biopsy or lysing peritubal adhesions. |
|