Colon
Appendectomy
Appendectomy
Using
the Linear Dissecting
Stapler
Transverse
Loop
Colostomy
End
Sigmoid Colostomy With Hartmann's Pouch
Closure
of a Loop
Colostomy
Anterior
Resection
of the Colon With Low
Anastomosis Using
the Gambee Suture
Technique
Low
Anastomosis
of Colon to Rectum
Using the End-to-End
Surgical Stapler
Technique
Anterior
Resection
of the Colon With
Low Anastomosis via
the Strasbourg-Baker
Technique |
End Sigmoid Colostomy
With Hartmann's Pouch
End sigmoid colostomy with a Hartmann's pouch is the
procedure of choice when permanent fecal diversion is required. In
some clinics, the distal portion of the rectosigmoid colon is exteriorized
as a mucous fistula in lieu of a Hartmann's pouch. The need for this
in colonic problems related to gynecologic oncology is rare.
Physiologic Change. In this operation, the fecal
stream is diverted from the rectum and anus. Compared with transverse
colostomy, end sigmoid colostomy gives additional length to the colon
for absorption of fecal fluid. Therefore, the stool is similar to that
passed per anum. End sigmoid colostomy offers an opportunity for colostomy
regulation that is generally not available in transverse colostomies.
A single stoma improves the fit of the colostomy bag and reduces skin
excoriation.
Points of Caution. An adequate incision
is needed to identify, mobilize, and open the mesentery of the sigmoid
colon. The incision should be selected to fit the needs of the individual
patient, ensuring proper placement of the colostomy stoma. The stoma
should not be placed in the patient's waistline, where clothing will
interfere with it, and should never be placed on the underside of a
large abdominal panniculus in obese patients. Several sutures placed
from the serosal surface of the bowel to the peritoneum will reduce
herniation and prolapse of the colon through the stoma.
Technique
The patient is placed in the supine position.
The abdomen is opened through a left paramedian or midline incision.
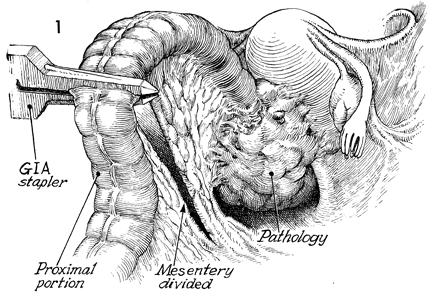
The sigmoid colon is identified, mobilized, and elevated. The
site for transection of the bowel is made on consideration of
the pathologic diagnosis. The mesentery is opened for approximately
8 cm. Often, the superior hemorrhoidal branch of the inferior
mesenteric artery must be clamped and divided, but the inferior
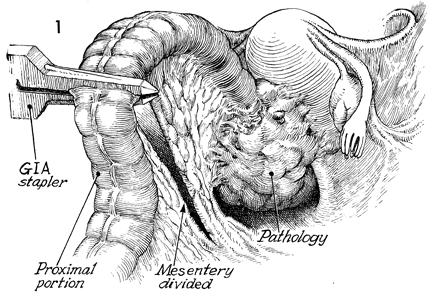
mesenteric artery itself is generally preserved. The gastrointestional
anastomosis (GIA) autosuture stapler is placed across the colon
and activated. |
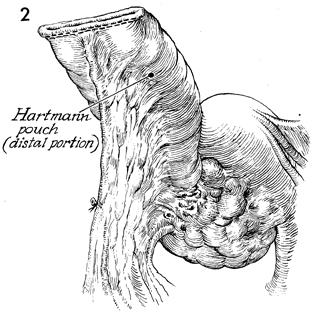
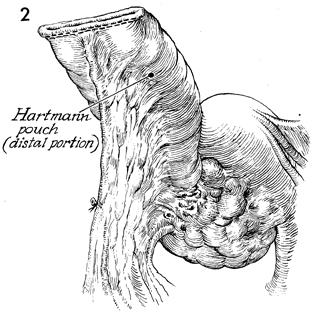
With the GIA stapler, the proximal
end of the distal segment of the colon (Hartmann's pouch) is
adequately closed. No further surgery to this segment is needed. |
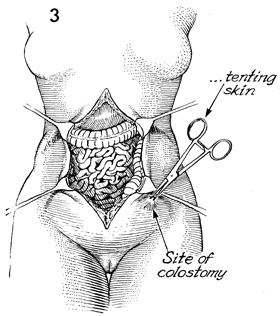
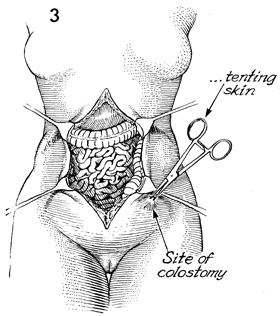
The appropriate site for the
colostomy stoma has been marked on the patient's abdomen with
indelible ink prior to surgery. An Allis clamp is placed on the
skin at this site and elevated. |
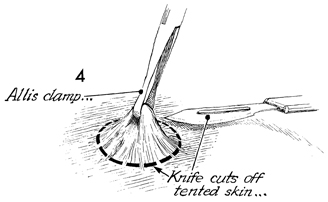
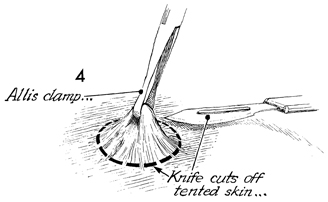
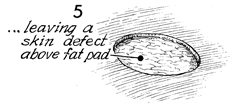
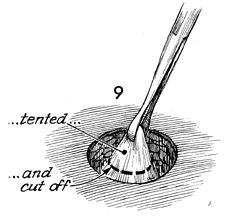
While the skin is held on
traction, a knife is used to remove a disc of skin and subcutaneous
tissue of appropriate diameter. |
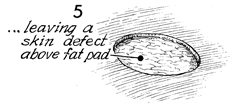
The skin disc has been removed. |
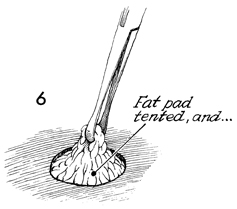
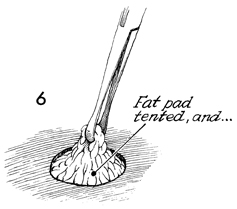
The subcutaneous fat is elevated
with an Allis clamp. |
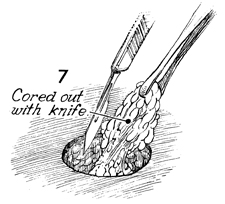
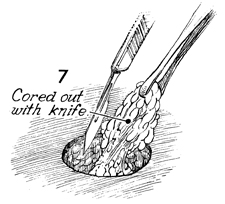
With the fat elevated, a knife is used to
remove the remaining fatty tissue, exposing the rectus fascia. |
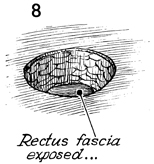
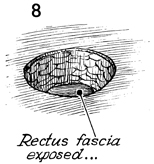
The rectus fascia is exposed. |
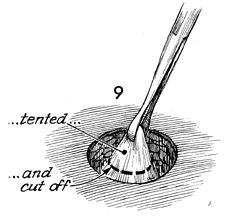
The rectus fascia is elevated with an Allis
clamp. A knife is used to remove a disc of rectus fascia 4 cm
diameter. |
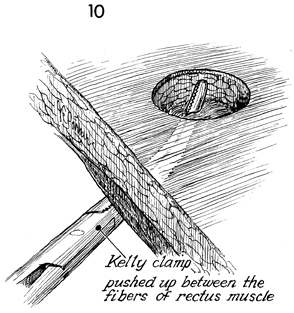
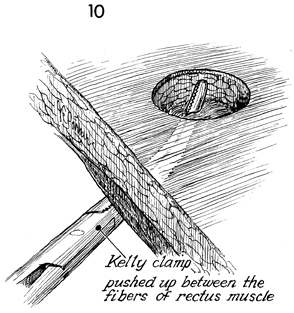
A large Kelly clamp is inserted through the
peritoneum, bluntly penetrating the fibers of the rectus muscle.
This incision is expanded with the Kelly clamp and fingers until
two fingers (4 cm) traverse the defect from the skin to peritoneum
without difficulty. |
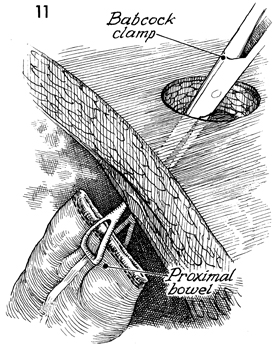
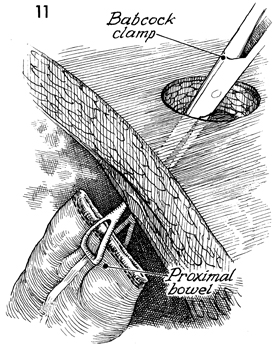
A Babcock clamp is inserted through the abdominal
wall defect. The distal segment of the descending colon is grasped. |
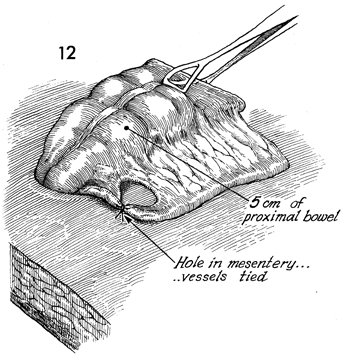
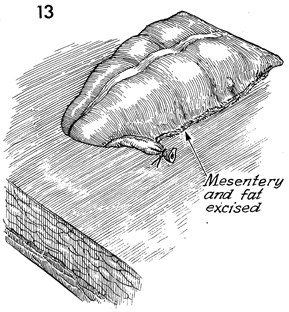
This distal segment of the descending colon
is pulled through the defect for a distance of approximately
7 cm. Excess fatty tissue on the mesenteric side of the colon
is clamped and tied up to but not exceeding 3 cm. |
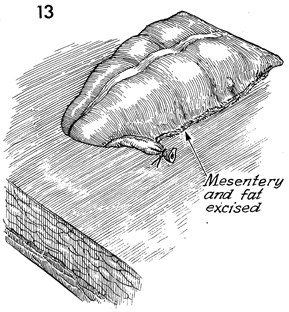
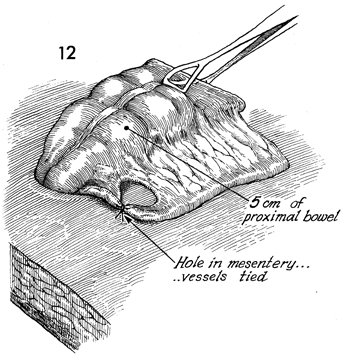
The excess fatty tissue is removed. The blood
supply of the colon is such that up to 5 cm of colon can be nourished
from the point of ligation of vessels in the mesentery. Colon
in excess of this amount may become ischemic and necrose. |
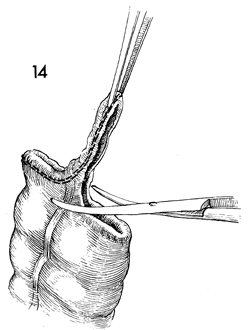
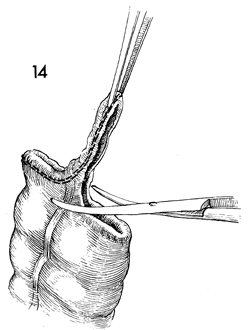
The stapled end of the proximal colon is
elevated with a forceps and resected with curved Mayo scissors. |
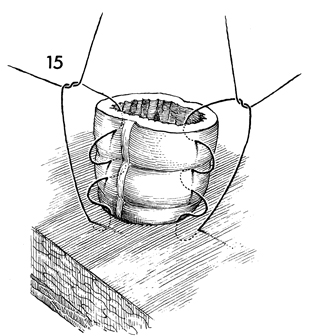
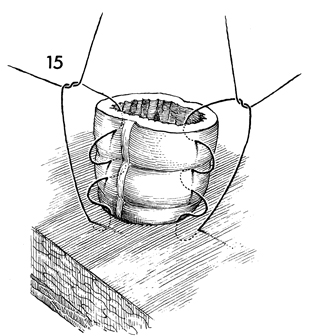
A "rosebud" stitch is utilized
to evert the colon onto the skin, thereby elevating it off the
skin edge by 1 1/2 cm. Elevating the stoma protects the skin
from fecal spillage. The stitch is started on the surface of
the skin 1 cm from the edge, goes through the epidermis and dermis,
is passed through the serosa and muscularis of the bowel wall,
and then transverses the edge of the bowel. |
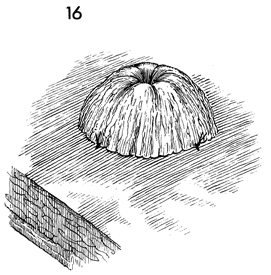
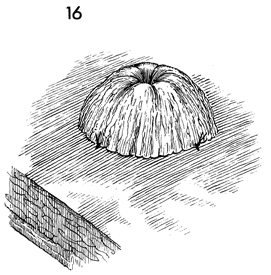
When tied, the stoma is inverted and raised
off the level of the skin. |
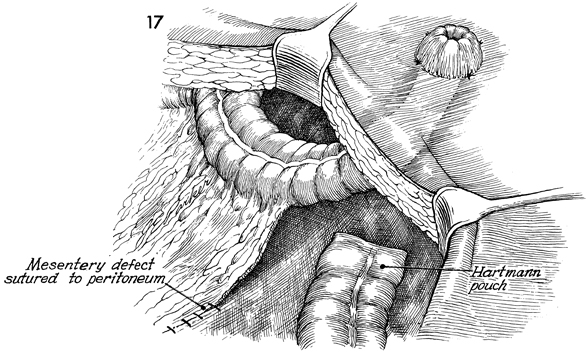
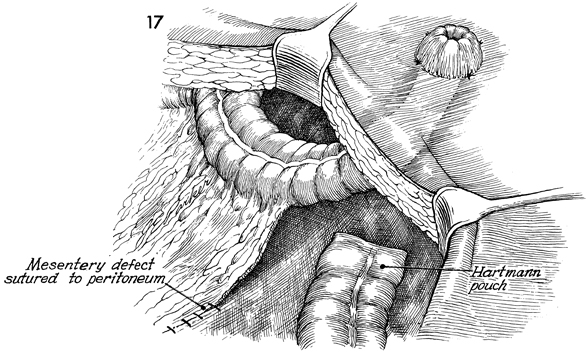
The mesentery of the large bowel is sutured
or stapled to the peritoneum to prevent internal hernia. |
|