Vagina
and Urethra
Anterior Repair and Kelly
Plication
Site Specific Posterior Repair
Sacrospinous
Ligament Suspension of the Vagina
Vaginal Repair of Enterocele
Vaginal Evisceration
Excision of
Transverse Vaginal Septum
Correction of
Double-Barreled Vagina
Incision
and Drainage of Pelvic Abscess via the Vaginal Route
Sacral Colpoplexy
Le Fort Operation
Vesicovaginal Fistula
Repair
Transposition
of Island Skin Flap for Repair of Vesicovaginal Fistula
McIndoe Vaginoplasty
for Neovagina
Rectovaginal Fistula
Repair
Reconstruction of
the Urethra
Marsupialization
of a Suburethral Diverticulum by the Spence Operation
Suburethral
Diverticulum via the Double-Breasted Closure Technique
Urethrovaginal
Fistula Repair via the Double-Breasted Closure Technique
Goebell-Stoeckel
Fascia Lata Sling Operation for Urinary Incontinence
Transection
of Goebell-Stoeckel Fascia Strap
Rectovaginal
Fistula Repair via Musset-Poitout-Noble Perineotomy
Sigmoid
Neovagina
Watkins Interposition Operation |
Sacral Colpopexy
Sacral colpopexy is a surgical procedure designed
for correction of prolapse of the vagina. It is an ideal procedure
for those women who are sexually active but who have total prolapse
of the vaginal canal. Prolapse of the vagina can occur following
a hysterectomy or with the uterus in place. If the uterus is still
in place and the patient is menopausal, it is best to remove it by
a hysterectomy (Uterus) prior to performing sacral colpopexy, unless
there are compelling reasons to leave it in situ. Sacral colpopexy
is an alternative procedure to sacrospinous ligament suspension of
the vagina (see Sacrospinous Ligament Suspension of the Vagina). In
some clinics, sacral colpopexy is reserved for those patients who have
recurrent prolapse following sacrospinous ligament suspension of the
vagina, since sacral colpopexy involves a pelvic laparotomy, whereas
the sacrospinous ligament suspension of the vagina can be performed
through the vagina. To date, there are no prospective, randomized studies
showing that one procedure is more efficacious than the other. Both
procedures have their advocates.
The strap material used in the sacral colpopexy varies.
There are some who prefer synthetic permanent mesh material made from
Prolene (Marlex and Mersilene). We prefer the patient's own fascia.
Our preference for the patient's own fascia (rectus fascia or fascia
lata) stems from our desire to avoid the sequelae of putting a foreign
body into or around the bacteria-contaminated vagina. The additional
effort to obtain fascia lata or rectus fascia is small compared to
the long-term sequelae of an infected foreign body.
Physiologic Changes. Vaginal
prolapse is an incapacitating and debilitating problem for women.
The exposed vaginal mucosa can become ulcerated with associated bleeding
and infections.
Replacing the vagina back into the pelvis in its proper anatomical
configuration is important. The normal vagina is shaped somewhat like
a backward hockey stick. The upper one-half to one-third of the vagina
should tilt posteriorly back upon the rectum. If the surgeon creates
a situation for the apex of the vagina to be in the midplane of the
pelvis, intra-abdominal pressure will produce recurrent prolapse.
Points of Caution. Sacral colpopexy is not a difficult
operation to perform. Several points need to be emphasized, however,
if the procedure is to be done successfully.
First, after entering the abdomen, identification of the right ureter
is vital. It should be mobilized and retracted laterally. The rectosigmoid
colon should also be mobilized and retracted laterally.
The vascular plexus on the periosteum of the sacrum can be associated
with copious bleeding if it is not properly managed.
The material used for the strap (natural fascia or
synthetic mesh) should be of the proper length and width to support
the apex of the vagina. The strap must be retroperitonealized and not
cross the pelvis like a "clothesline." Such a situation is an invitation
to internal herniation and incarceration of the small bowel, leading
to obstruction and necrosis.
Technique
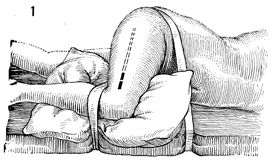
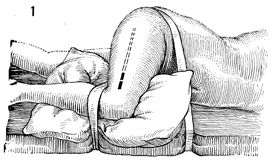
For the surgeon to harvest the fascia
lata, the patient is placed in the lateral decubitus position
with flexion of both the hips and knees at approximately 60°.
A pillow should be placed between the knees to abduct the thigh
until it is level. Two large pieces of tape are used to stabilize
the patient and prevent her from moving to either side. The lateral
thigh is prepped and draped. The solid line marks the
site of the initial incision, and the dotted line marks
the direction of the tunneled Masson fascia stripper. |
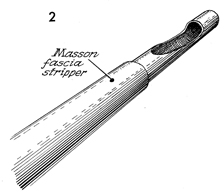
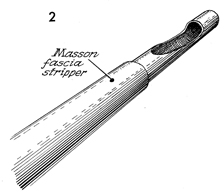
The Masson fascia stripper consists
of two hollow metal tubes-one inside, one outside. The inner
tube has a narrow opening, "the eye," near one end; the edge
of the outer tube is sharpened to allow cutting of the fascia
strip at the desired level. |
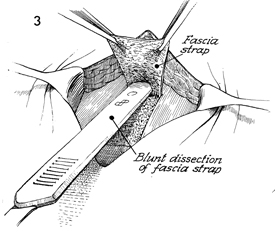
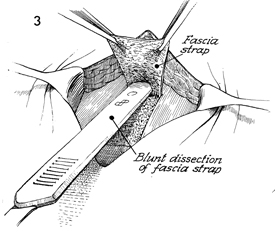
The incision is open; the base of
the fascia strap is started by hand with a scalpel. The handle
of the scalpel is used to perform blunt dissection of the fascia
strap off its bed. The finger is used to tunnel underneath the
subcutaneous fat on top of the fascia. The base of the strap
should be 4 cm wide. At least 6 cm of the strap should be taken
by the knife before applying the Masson stripper. |
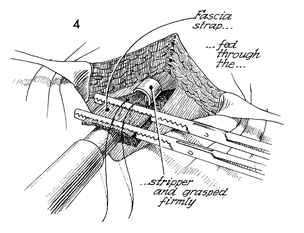
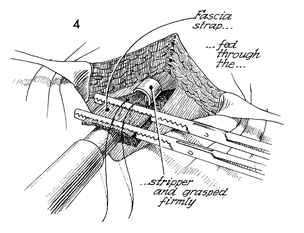
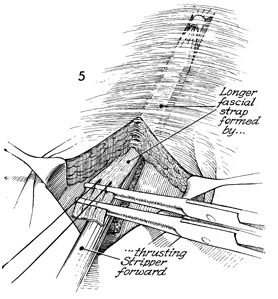
The Masson fascia stripper is moved
into position. The strap that has been formed by sharp dissection
is placed through the opening of the fascia stripper. Two straight
Kocher clamps are placed across the strap, and a suture is placed
adjacent to the Kocher clamps as a safety suture to retrieve
the strap if it breaks and retracts up the thigh. |
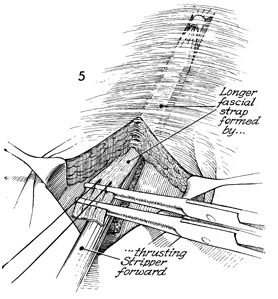
The surgeon retracts the Kocher
clamps caudally as the Masson fascia stripper is advanced cephalad.
A point is reached where the Masson fascia stripper will advance
no farther. At that point, the surgeon unscrews the handle of
the Masson fascia stripper and evulses the strap. The strap is
brought out through the leg wound. |
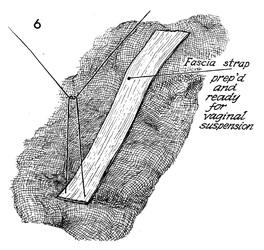
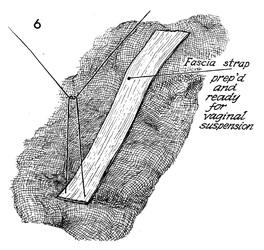
The fascia strap is shown. The suture
at the end of the strap is removed. |
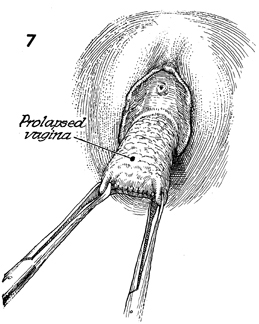
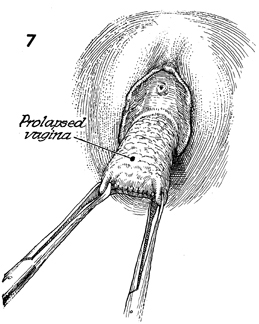
The patient is changed to the dorsal
lithotomy position. The prolapsed vagina is noted. Two Allis clamps
are placed on the vaginal apex. If a hysterectomy has previously
been performed, the suture line will be noted in the vaginal apex. |
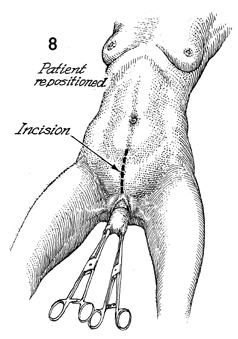
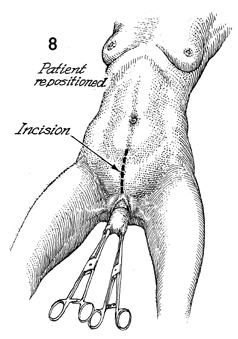
A midline incision-Pfannenstiel or midline-is
made. The peritoneal cavity is entered. |
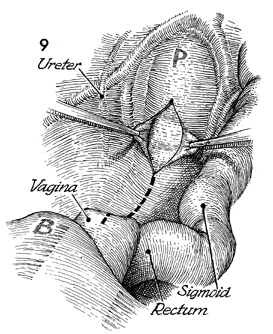
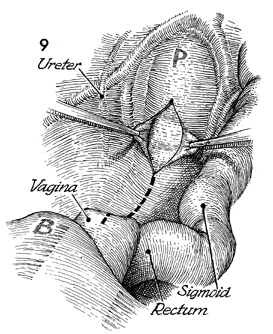
After packing the bowel away with moist gauze,
the surgeon identifies the right ureter and the rectosigmoid
colon. An incision is made in the posterior peritoneum from the
sacral promontory (P). This incision is carried down
over the cul-de-sac and the vaginal apex. The vagina is replaced
into the abdominal cavity by either a 4-cm obturator or a sponge
stick held in an ovum forceps. |
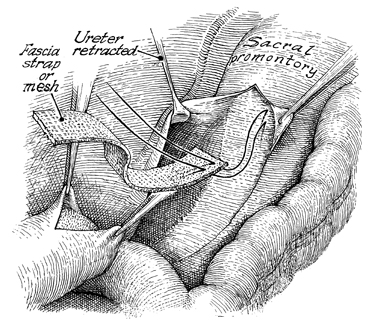
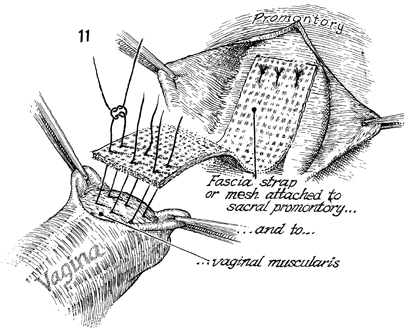
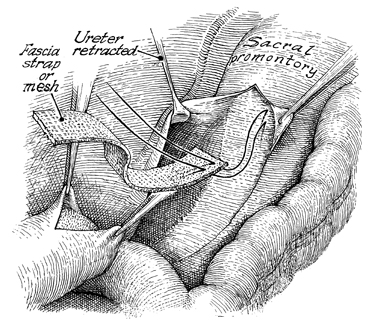
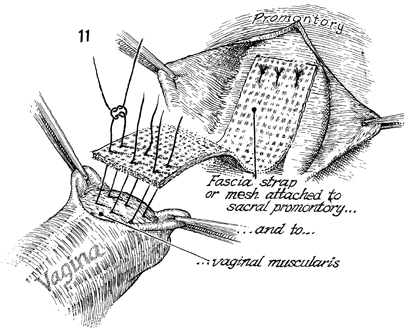
The fascia strap is sutured
to the periosteum of the sacrum. Sutures should be placed into
the periosteum of the sacrum and then brought through the fascia
as shown here. Three to four sutures are placed. The distal
end of the strap is sutured to the apex of the vagina. Three
sutures are placed in the anterior vaginal wall with interrupted
synthetic permanent sutures. The strap is placed over the dome
of the vagina, and additional sutures are applied if needed.
The cul-de-sac is obliterated by suturing the uterosacral ligaments
in the midline. |
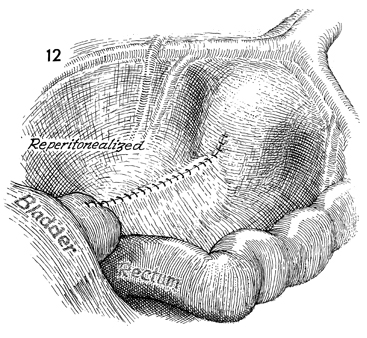
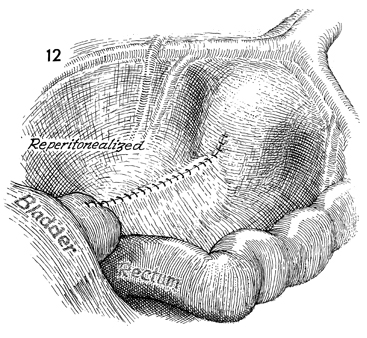
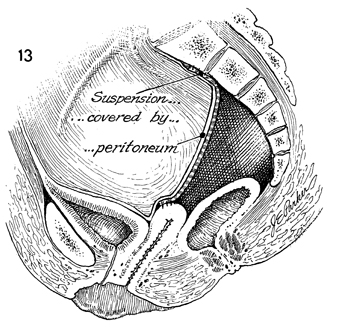
The peritoneum is sutured over
the strap to reperitonealize the pelvis and prevent the "clothesline"
effect. |
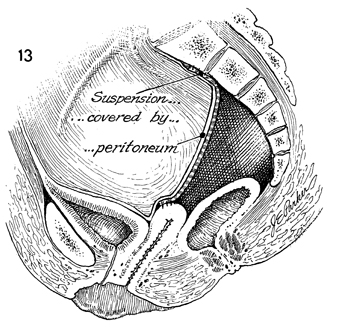
A sagittal view shows the suspension covered
by the peritoneum. The strap is sutured to the periosteum of
the sacrum and ultimately over the dome of the vaginal apex.
The vagina should lie posteriorly over the rectosigmoid colon. |
|