Fallopian
Tubes
and Ovaries
Laparoscopy
Technique
Diagnostic
Uses
of Laparoscopy
Demonstration
of Tubal Patency
via Laparoscopy
Laparoscopic
Resection
of Unruptured
Ectopic Pregnancy
Ovarian
Biopsy
via Laparoscopy
Electrocoagulation
of
Endometriosis via
Laparoscopy
Lysis
or Adhesions
via Laparoscopy
Control
of Hemorrhage
During Laparoscopy
Fallopian
Tube
Sterilization
Sterilization
by
Electrocoagulation and
Division via Laparoscopy
Silastic
Band Sterilization
via Laparoscopy
Hulka
Clip Sterilization
via Laparoscopy
Sterilization
by the
Pomeroy Operation
Sterilization
by the
Modified Irving Technique
Sterilization
by the
Minilaparotomy Technique
Sterilization - Ucheda Technique
Salpingectomy
Salpingo-oophorectomy
Fimbrioplasy
Tuboplasty
-
Microresection
and Anastomosis
of the Fallopian Tube
Wedge
Resection
of the Ovary
Torsion
of the Ovary
Ovarian
Cystectomy |
Diagnostic Uses of Laparoscopy
Laparoscopy offers the pelvic surgeon a significant advantage by providing
accurate diagnostic techniques without requiring exploratory laparotomy.
It is particularly useful in (1) identifying unique and unusual alterations
in pelvic anatomy, (2) resolving questions about an ectopic pregnancy
that is difficult to diagnose. (3) differentiating between borderline
and severe cases of pelvic inflammatory disease and between pelvic
disease and acute appendicitis, and (4) evaluating the pelvis and Fallopian
tubes in cases of infertility.
The purpose of the operation is to visualize the lower abdomen and
pelvis without performing a laparotomy.
Physiologic Changes. None.
Points of Caution. Laparoscopy should not be used
diagnostically where there is overwhelming evidence of pelvic disease
requiring exploratory laparotomy. For example, it is unwise and contraindicated
to perform diagnostic laparoscopy where there are pelvic masses greater
than 14 weeks gestation size. In these cases, exploratory laparotomy
should be performed. Likewise, diagnostic laparoscopy should not be
performed with a gross hemoperitoneum or generalized abdominal peritonitis.
Performance of laparoscopy is not excessively hazardous under these
conditions, but it adds nothing to the overall diagnosis and simply
delays exploratory laparotomy.
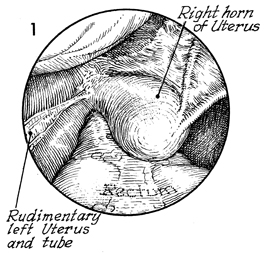
Technique
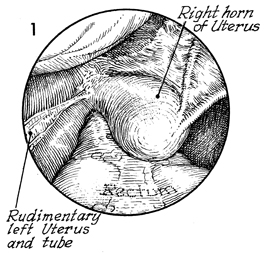
An alteration in pelvic anatomy
that may be associated with a congenital anomaly of the Mullerian
duct is shown. In institutions with adequate cytogenic laboratories,
diagnostic laparoscopy is not required for anomalies of the internal
genitalia because in most cases the anomaly can be diagnosed
without operative intervention. In cases of failure in Mullerian
duct fusion in which there is a rudimentary or smaller separate
horn on one side and an enlarged horn on the opposite side, however,
the use of the laparoscope may be valuable in developing a complete
treatment plan. |
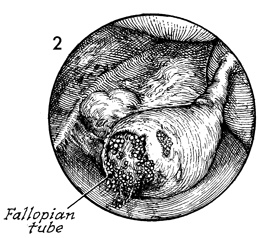
Women with amenorrhea, abdominal
pain, vaginal bleeding, and/or an adnexal mass do not need diagnostic
laparoscopy to rule out the possibility of ectopic pregnancy.
However, many women with ectopic pregnancy have vague symptoms
and ambiguous signs. Even if a culdocentesis shows a small amount
of nonclotting blood, the laparoscope is a valuable instrument
in differentiating a tubular pregnancy from a bleeding corpus
luteum cyst. In addition, the bleeding corpus luteum can be electrocoagulated
through the laparoscope, and laparotomy may be avoided. If there
is gross abdominal distention from a hemoperitoneum, however,
laparoscopy only delays appropriate therapy.
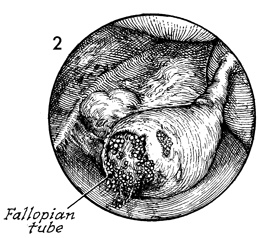
Frequently, the surgeon is not
able to see the dilated Fallopian tube containing the pregnancy
as shown here. Often, a cornual mass is visible, consisting of
clotted blood mixed with tissue. |
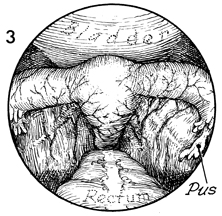
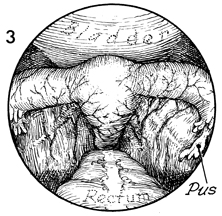
Diagnostic laparoscopy has been of great
assistance in differentiating between the difficult cases of
pelvic inflammatory disease and acute appendicitis. The treatment
for each is quite different, and if an accurate preoperative
diagnosis can be made, substantial savings in hospital costs
and utilization of hospital beds can be made. In addition, purulent
material can be aspirated through the laparoscope to ascertain
the exact etiology of the endosalpingitis and aid in selection
of appropriate antibiotic therapy. When there are signs and symptoms
of generalized peritonitis, however, laparoscopy is contraindicated
and only delays the exploratory laparotomy needed to correct
the problem. |
|
|