Malignant
Disease:
Special Procedures
Staging
of Gynecologic
Oncology Patients With
Exploratory Laparotomy
Subclavian Port-A-Cath
Peritoneal Port-A-Cath
Application
of Vaginal
Cylinders for Intracavitary
Radiation Therapy
Application
of Uterine Afterloading Applicators
for Intracavitary Radiation Therapy
Pelvic High-Dose
Afterloader
Abdominal
Injection of Chromic Phosphate
( ) )
Supracolic
Total Omentectomy
Omental Pedicle "J"
Flap
Tube Gastrostomy
Total Vaginectomy
Radical
Vulvectomy
With Bilateral Inguinal
Lymph Node Dissection
Reconstruction
of the
Vulva With Gracilis Myocutaneous Flaps
Transverse
Rectus
Abdominis Myocutaneous
Flap and Vertical Rectus
Abdominis Myocutaneous
Flap
Radical
Wertheim
Hysterectomy With
Bilateral Pelvic Lymph
Node Dissection and With Extension of the Vagina
Anterior Exenteration
Posterior Exenteration
Total Pelvic
Exenteration
Colonic
"J" Pouch Rectal
Reservoir
Kock Pouch
Continent Urostomy
Omental "J" Flap
Neovagina
Ileocolic
Continent Urostomy (Miami Pouch)
Construction
of Neoanus
Gracilis Dynamic Anal
Myoplasty
Skin-Stretching
System Versus Skin Grafting
Gastric
Pelvic Flap for
Augmentation of Continent Urostomy or Neovagina
Control
of Hemorrhage in Gynecologic Surgery
Repair
of the Punctured
Vena Cava
Ligation
of a Lacerated
Internal Iliac Vein and
Suturing of a Lacerated Common Iliac Artery
Hemorrhage
Control in
Sacrospinous Ligament
Suspension of the Vagina
Presacral
Space
Hemorrhage Control
What
Not to Do in Case of Pelvic Hemorrhage
Packing
for Hemorrhage
Control
Control
of Hemorrhage
Associated With Abdominal Pregnancy |
Total Vaginectomy
Total vaginectomy is indicated for malignant
disease of the vagina. It is frequently required in combination with
total abdominal hysterectomy or radical Wertheim hysterectomy. It
is the only alternative after total pelvic irradiation for recurrent
microinvasive carcinoma of the vagina. The planes of dissection after
irradiation are difficult, and there is a high risk of vesicovaginal
and rectovaginal fistula. Preoperatively, the surgeon should advise
the patient with regard to replacement of the vagina with a skin
graft, and a preoperative plan should be made as the patient's sexual
status indicates. Although the vagina is occasionally removed abdominally,
the procedure is best initiated from the vaginal route. Frequently,
an abdominoperitoneal approach is used because the operation is combined
with either a radical hysterectomy or simple hysterectomy.
The
purpose of the operation is to remove the vagina.
Physiologic Changes. If only the vagina is removed
and no opening is made into the bladder or rectum, there is little
physiologic change.
Points of Caution. The major complication
of this operation, particularly after pelvic irradiation, is inadvertent
vesicovaginal or rectovaginal fistula formation. Therefore, the dissection
should be carried out in the most meticulous manner possible. If the
surgeon can dissect within a plane outside the pubovesical cervical
fascia, fistula formation will be reduced.
Meticulous hemostasis should
be performed prior to introducing the split-thickness skin graft.
Technique
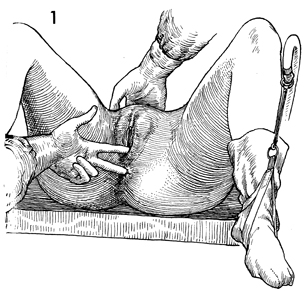
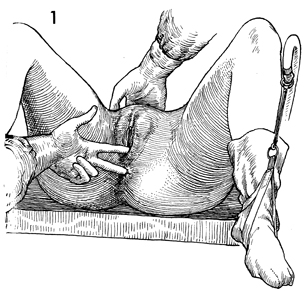
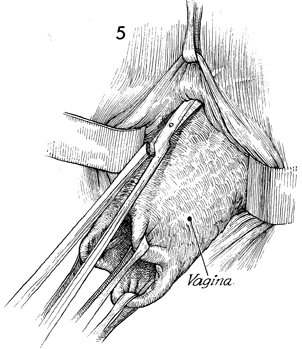
The patient is placed in the dorsal lithotomy
position with her buttocks off the end of the table by approximately
8 cm. Adequate vaginal and pelvic examinations are performed,
and appropriate biopsies are taken. The bladder is emptied by
catheter drainage. |
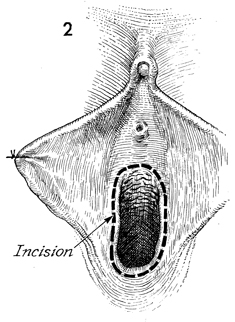
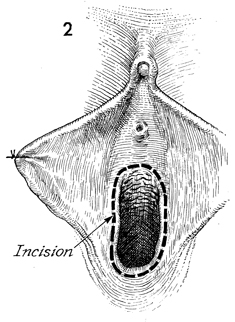
An incision is made around the circumference
of the vaginal vault down to the pubocervical fascia underneath
the urethra and the perirectal fascia overlying the rectum. |
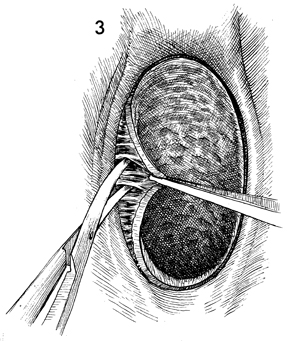
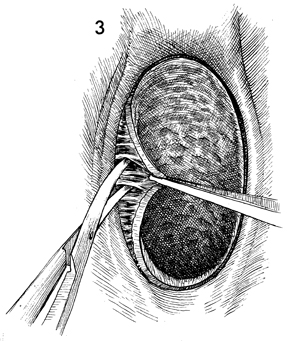
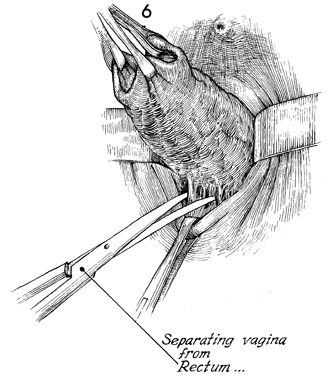
Since blood supply to the vagina comes predominantly
from the lateral side, dissection is begun there first. The vaginal
epithelium is deviated to the midline, and Metzenbaum scissors
are used to dissect the vaginal mucosa from its lateral wall. |
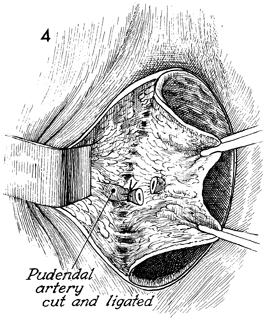
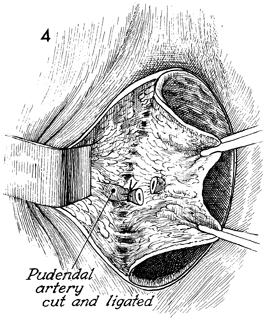
Care is taken to identify
the vaginal branches of the pudendal artery, which should be
securely clamped and tied. |
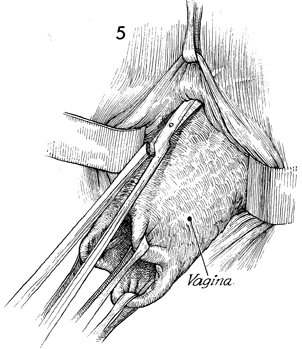
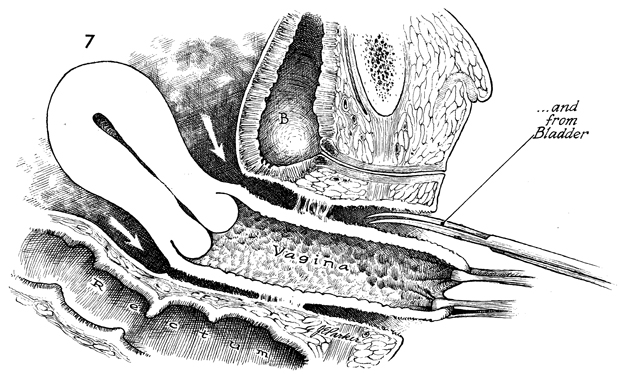
Dissection underneath the urethra and bladder
is generally bloodless as long as it is confined to the plane
between the vaginal mucosa and the pubovesical cervical fascia.
If the pubovesical cervical fascia becomes involved, the small
vessels in the bladder wall make hemostasis difficult. |
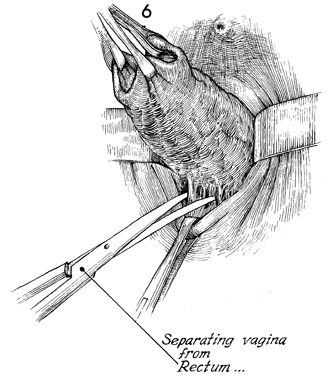
The dissection posteriorly
should be performed in the plane above the perirectal fascia,
or copious bleeding can occur from the hemorrhoidal plexus of
vessels. |
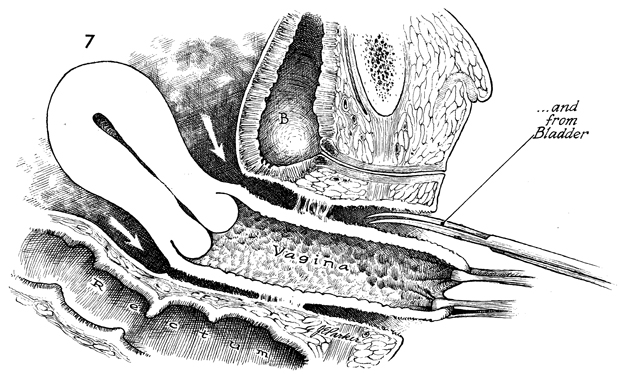
When the dissection has reached
the cul-de-sac posteriorly and the vesicouterine peritoneal area
anteriorly, the vagina can be removed by itself, but it is generally
removed in conjunction with total abdominal hysterectomy. The
vaginal canal must then be managed according to the sexual needs
of the patient.
If the patient is sexually active,
a skin graft can be placed after meticulous hemostasis has been
achieved (see Vagina and Urethra on McIndoe Vaginoplasty), or
the vaginal canal can be closed by suturing the pubovesical cervical
fascia to the rectal fascia posteriorly (see Vagina and Urethra
on the Le Fort operation). If a McIndoe vaginoplasty is to be
performed, suction catheters should be left in the pelvic area
and brought out through left and right lower quadrant stab wounds;
or if closure of the vaginal space is indicated as in the Le
Fort operation, they can be brought out through the lateral vaginal
vault. A suprapubic Foley catheter is left in the bladder until
voiding is established. B,
bladder. |
|