Malignant
Disease:
Special Procedures
Staging
of Gynecologic
Oncology Patients With
Exploratory Laparotomy
Subclavian Port-A-Cath
Peritoneal Port-A-Cath
Application
of Vaginal
Cylinders for Intracavitary
Radiation Therapy
Application
of Uterine Afterloading Applicators
for Intracavitary Radiation Therapy
Pelvic High-Dose
Afterloader
Abdominal
Injection of Chromic Phosphate
( ) )
Supracolic
Total Omentectomy
Omental Pedicle "J"
Flap
Tube Gastrostomy
Total Vaginectomy
Radical
Vulvectomy
With Bilateral Inguinal
Lymph Node Dissection
Reconstruction
of the
Vulva With Gracilis Myocutaneous Flaps
Transverse
Rectus
Abdominis Myocutaneous
Flap and Vertical Rectus
Abdominis Myocutaneous
Flap
Radical
Wertheim
Hysterectomy With
Bilateral Pelvic Lymph
Node Dissection and With Extension of the Vagina
Anterior Exenteration
Posterior Exenteration
Total Pelvic
Exenteration
Colonic
"J" Pouch Rectal
Reservoir
Kock Pouch
Continent Urostomy
Omental "J" Flap
Neovagina
Ileocolic
Continent Urostomy (Miami Pouch)
Construction
of Neoanus
Gracilis Dynamic Anal
Myoplasty
Skin-Stretching
System Versus Skin Grafting
Gastric
Pelvic Flap for
Augmentation of Continent Urostomy or Neovagina
Control
of Hemorrhage in Gynecologic Surgery
Repair
of the Punctured
Vena Cava
Ligation
of a Lacerated
Internal Iliac Vein and
Suturing of a Lacerated Common Iliac Artery
Hemorrhage
Control in
Sacrospinous Ligament
Suspension of the Vagina
Presacral
Space
Hemorrhage Control
What
Not to Do in Case of Pelvic Hemorrhage
Packing
for Hemorrhage
Control
Control
of Hemorrhage
Associated With Abdominal Pregnancy |
Skin-Stretching System
Versus Skin Grafting
Skin grafting has been an unusual but needed procedure in gynecologic
oncology surgery. The physiology of wound healing is dramatically improved
if wounds are covered as soon as possible and not left granulating
over a period of months.
A new instrument has been added to the gynecologic surgeons armamentarium,
the skin-stretching devise known as Sure-Closure (MedChem, Woburn,
Massachusetts).
The purpose of the operation is to cover an exposed defect on the abdominal
wall, vulva, or sacrum.
Physiologic Changes. The predominate physiologic
change is closure of the wound to prevent contraction and epithelialization.
Loss of fluid and protein from open wounds allowed to granulate over
a period of time is a major metabolic and nutritional problem.
Points of Caution. Care
must be taken to adequately mobilize the edges of the wound. The
wound should never be covered under tension.
The air dermatome should be held at an angle of 45-60°. Holding the
air dermatome at an angle of less than 45° produces (1) a split-thickness
skin graft that is chopped into pieces and (2) a donor site with an
irregular surface.
The technique of skin-stretching via the device known
as Sure-Closure takes advantage of the processes of the "mechanical
creeping" produced by the Sure-Closure device, which applies a controlled
amount of tension evenly along two open wound margins of skin. The
mechanical stretcher uses the vesicoelastic properties of skin to stretch
in a reasonable time while minimizing the skins tendency to recoil.
Repeated cycles of stretching are performed over 30-40 minute period
of time until the skin margins can be brought in opposition for suturing
without tension.
Technique
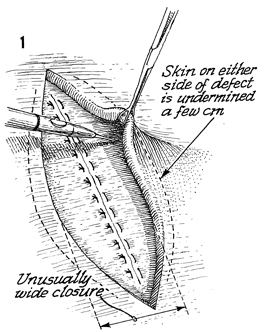
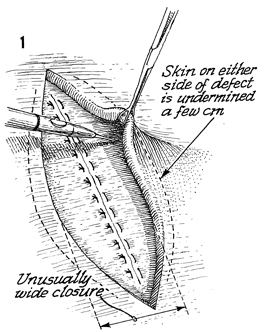
In an open wound of the abdominal wall with
the underlying rectus fascia closed with interrupted sutures,
the skin on either side of the defect is undermined for 2-3 cm
with the electrocoagulation device. |
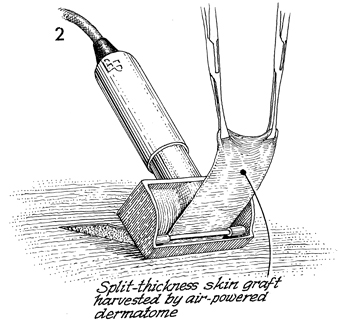
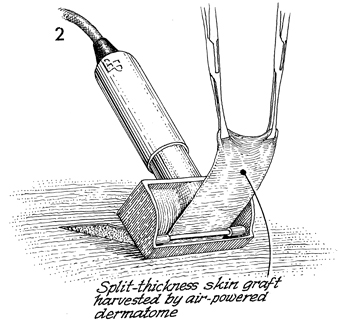
An air dermatome is demonstrated taking a
split-thickness skin graft. Note that the dermatome occupies
a 45° angle to the level of the donor site. The graft is grasped
with Allis forceps or skin hooks. The air dermatome is set to
produce a graft of 0.2 cm.
The donor site is covered with
a fine mesh gauze to prevent epithelial cells from growing through
the pores on regular gauze, debriding the donor wound with each
dressing change. |
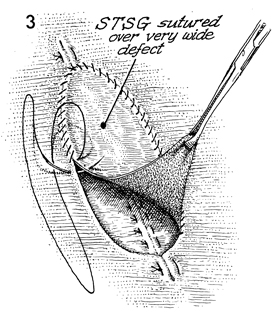
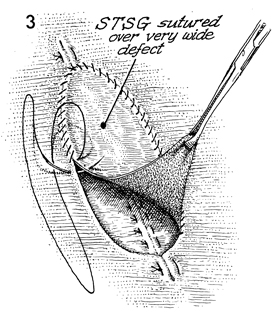
The graft is laid on the open wound, and
the margins of open wound are sutured to the margins of the split-thickness
graft (STSG). |
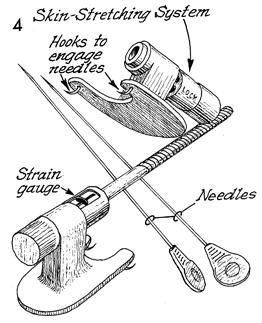
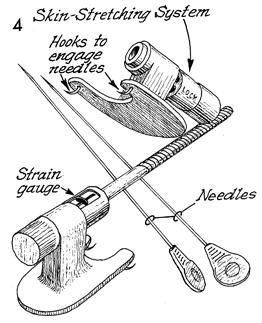
The elements of the Sure-Closure
skin-stretching system can be seen here. They consist of two
straight needles, the two parts of the stretching device with
hooks that engage the two needles under the platform of the stretching
device. On one stretching device there is a strain gauge that
prevents the skin from stretching too rapidly. The upper platform
of the stretching device shows the needles but also shows the
locking system that prevents the device from unlocking after
the skin has been stretched. |
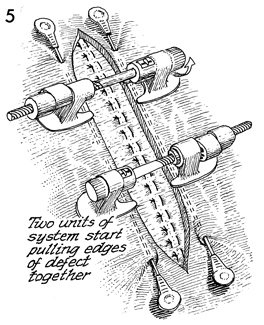
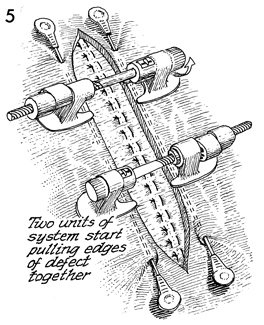
The needles have been inserted along the
margins of the skin parallel to the wound. The stretching system
has small retained needles on the bottom of their platforms stuck
under the linear needles to provide a solid stretching system.
The strain gauge portion of the stretching system is engaged
into the receiving end and locked in place. The wheel screw of
the stretching system is turned, and the margins of the skin
are stretched. The strain gauge will show when the skin is being
stretched beyond its capacity. There is a clutch in the stretching
system that disengages the wheel crank when too much stretching
pressure has been applied to the skin; this allows for the skin
to recover before further stretching is allowed. |
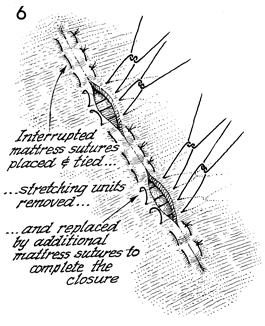
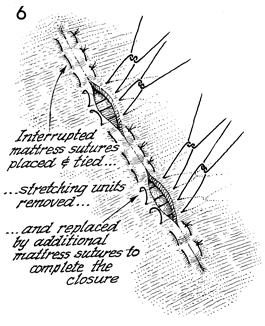
When the margins of the wound
have been approximated to each other, the wound is closed with
interrupted mattress sutures. |
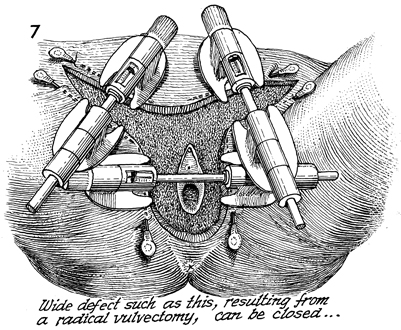
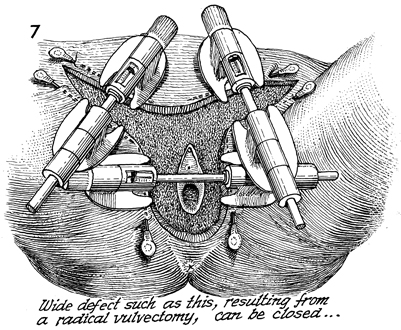
The devices have been set in place for a
radical vulvectomy incision. After stretching, tension has been
removed from the skin of the inguinal node dissection. The skin
of the vulva resection can be stretched to close the skin to
the margins of the vagina without tension through the skin-stretcher
process. |
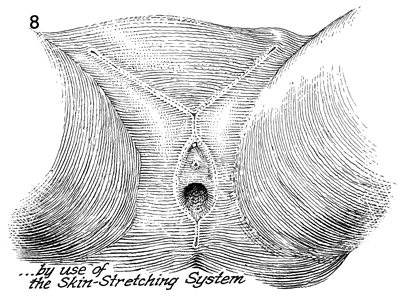
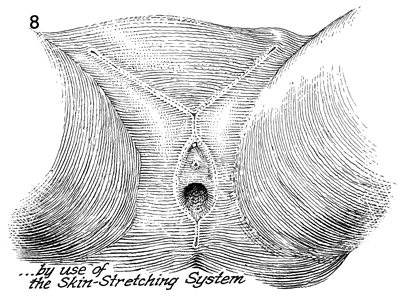
The wound is closed following the stretching
process. |
|