Malignant
Disease:
Special Procedures
Staging
of Gynecologic
Oncology Patients With
Exploratory Laparotomy
Subclavian Port-A-Cath
Peritoneal Port-A-Cath
Application
of Vaginal
Cylinders for Intracavitary
Radiation Therapy
Application
of Uterine Afterloading Applicators
for Intracavitary Radiation Therapy
Pelvic High-Dose
Afterloader
Abdominal
Injection of Chromic Phosphate
( ) )
Supracolic
Total Omentectomy
Omental Pedicle "J"
Flap
Tube Gastrostomy
Total Vaginectomy
Radical
Vulvectomy
With Bilateral Inguinal
Lymph Node Dissection
Reconstruction
of the
Vulva With Gracilis Myocutaneous Flaps
Transverse
Rectus
Abdominis Myocutaneous
Flap and Vertical Rectus
Abdominis Myocutaneous
Flap
Radical
Wertheim
Hysterectomy With
Bilateral Pelvic Lymph
Node Dissection and With Extension of the Vagina
Anterior Exenteration
Posterior Exenteration
Total Pelvic
Exenteration
Colonic
"J" Pouch Rectal
Reservoir
Kock Pouch
Continent Urostomy
Omental "J" Flap
Neovagina
Ileocolic
Continent Urostomy (Miami Pouch)
Construction
of Neoanus
Gracilis Dynamic Anal
Myoplasty
Skin-Stretching
System Versus Skin Grafting
Gastric
Pelvic Flap for
Augmentation of Continent Urostomy or Neovagina
Control
of Hemorrhage in Gynecologic Surgery
Repair
of the Punctured
Vena Cava
Ligation
of a Lacerated
Internal Iliac Vein and
Suturing of a Lacerated Common Iliac Artery
Hemorrhage
Control in
Sacrospinous Ligament
Suspension of the Vagina
Presacral
Space
Hemorrhage Control
What
Not to Do in Case of Pelvic Hemorrhage
Packing
for Hemorrhage
Control
Control
of Hemorrhage
Associated With Abdominal Pregnancy |
Transverse Rectus Abdominis
Myocutaneous Flap
and Vertical
Rectus Abdominis Myocutaneous Flap
Muscle flaps play a large role in pelvic reconstruction of the female
patient who has had radical resection for malignant disease, particularly
when associated with total pelvic irradiation. They offer the advantage
of bringing a non-irradiated tissue with a non-irradiated blood supply
into the pelvis for coverage of defects. The rectus abdominis muscle
with its unique blood supply coming from the inferior epigastric vessels,
right or left, and the anatomy of the vessels in the rectus abdominis
muscle allow a muscle flap to be based on a long muscle pedicle with
excellent blood supply. The transverse rectus abdominis myocutaneous
(TRAM) flap and the vertical rectus abdominis myocutaneous (VRAM) flap
have the smallest incidence of necrosis of any of the myocutaneous
flaps associated with pelvic reconstructive surgery.
Physiologic Changes. The physiologic change is that
an open wound has been covered with a myocutaneous or muscle flap that
offers an excellent covering for a wound and, at the same time, brings
in a muscle with an excellent blood supply, i.e., the inferior epigastric
artery, a branch of the external iliac artery.
Points of Caution. The paddle-shaped skin flap should
not be separated from the anterior rectus fascia in order to preserve
the perforator vessels from the muscle to the skin. Extreme care should
be taken to ensure the integrity of the inferior epigastric vessels
as they branch off the external iliac vessels. When the neurovascular
bundle of the inferior epigastric artery has been interrupted, it would
be extremely unusual for the VRAM flap to survive.
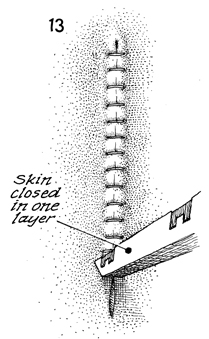
Technique
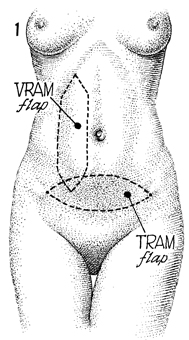
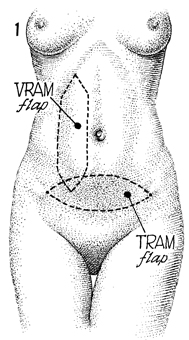
The abdominal wall shows the VRAM flap and
the TRAM flap. |
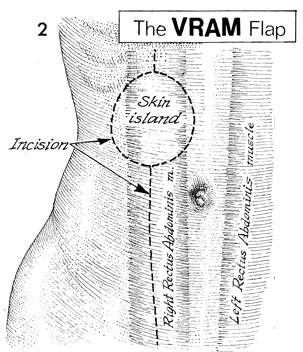
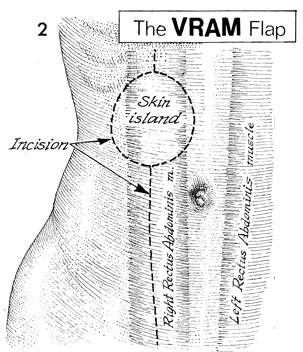
The VRAM flap is outlined. The rectus abdominis
muscles are seen ghosted beneath the skin. The incision is noted.
The skin island is designed appropriate to the defect to be filled
within the pelvis. |
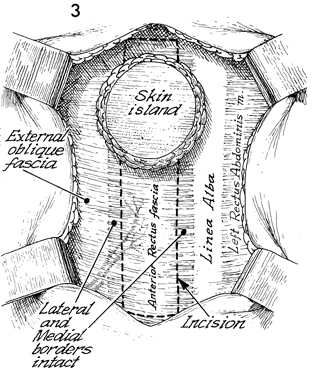
After the incision has been made along the
medial border of the rectus fascia and the skin island is noted
toward the superior portion of the proposed flap, the external
oblique fascia, the lateral and medial borders of the fascia,
is noted. The linea alba is seen. The left rectus abdominis muscle
is ghosted under the rectus fascia. The incision follows a second
incision in the rectus fascia and is outlined as above, keeping
intact a 5-cm width of rectus fascia to be taken with the flap.
This ensures that the perforators coming off the anterior surface
of the muscle through the rectus fascia are not interrupted or
damaged. The inferior epigastric vessels are shown ghosted on
the lateral portion of the rectus muscle. |
|
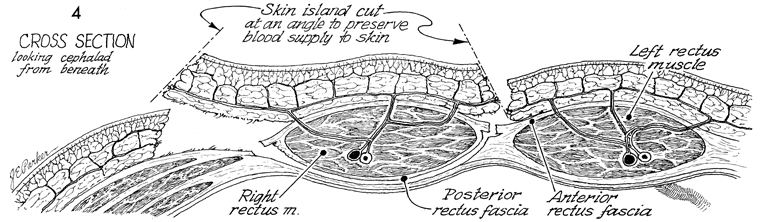 |
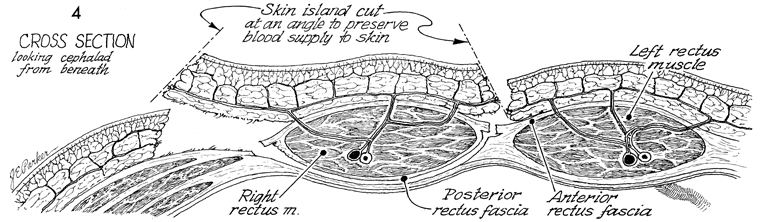
A cross section looking cephalad from beneath
the flap is shown. The skin island is cut at an angle to preserve
blood supply to the surface of the skin. The rectus muscles are
shown. The posterior rectus fascia is left intact; the muscle
is dissected off the posterior rectus fascia. By not sacrificing
the posterior rectus fascia, reduction in hernias is noted. |
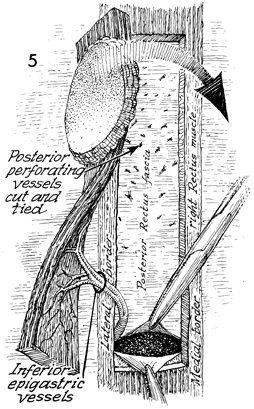
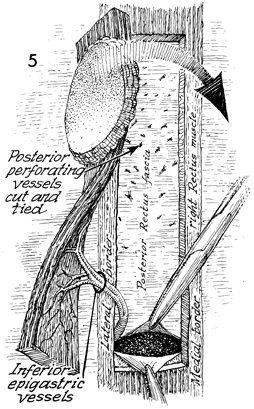
The VRAM flap has been completed, the posterior
rectus fascia is noted, and the small perforators coming off
the posterior rectus fascia are ligated. The rectus muscle is
transected at the pubic symphysis area. The entire muscle with
its sheath of rectus abdominal fascia on the anterior portion
of the muscle is intact. The skin island is now ready for rotation
through the defect made in the posterior rectus fascia above
the symphysis pubis to bring this into the pelvic area. The medial
border of the right rectus muscle has been shown. The lateral
border of the right rectus fascia is also noted. |
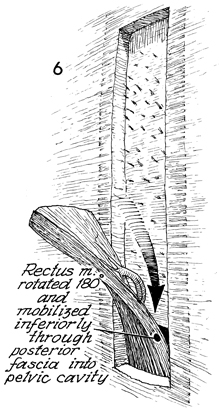
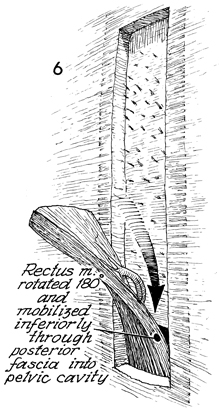
The entire rectus muscle
is lifted out of its fascia covering then rotated 180° and mobilized
inferior through the posterior fascia into the pelvic cavity.
The blood supply is coming exclusively through the inferior epigastric
artery, and the perforators are coming through the muscles as
shown in Figure 4. |
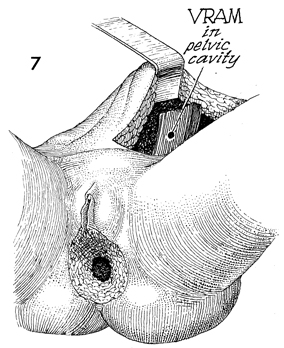
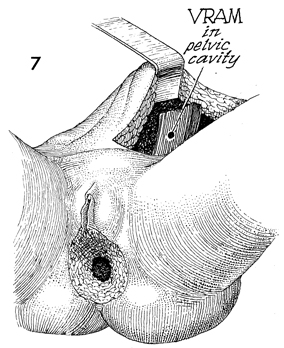
The VRAM flap is now pulled through the abdominal
cavity into the pelvis and will be brought out to cover the vulvoanal
defect noted in this particular patient. Modifications can be
made to cover the exact limits of the defect noted in specific
patients. |
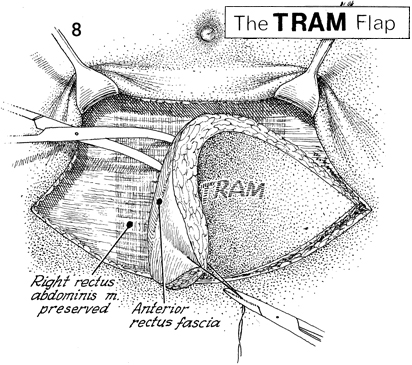
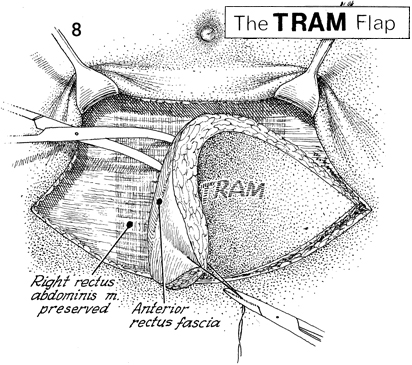
The TRAM flap is made in a paddle-shaped
manner from one anterior superior iliac spine to the opposite
anterior superior iliac spine. The rectus abdominis muscle can
be seen beneath the rectus fascia. Note that the right rectus
abdominis muscle has been preserved in this particular case.
The dissection is made underneath the anterior rectus fascia,
which is preserved in a transverse fashion. |
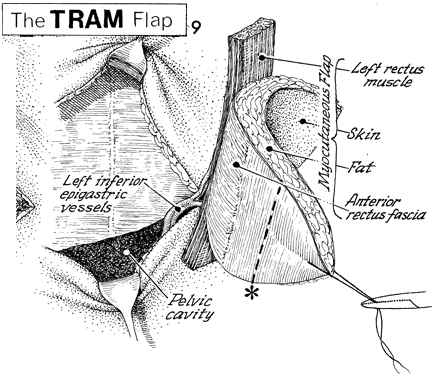
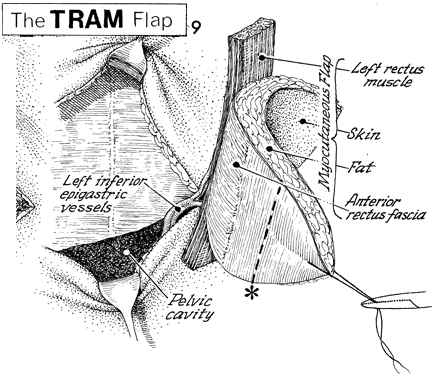
The TRAM flap is supported by
the left inferior epigastric muscles. Note that the left rectus
muscle has been brought out of its fascia enclosure, preserving
the anterior rectus fascia for 5 cm on each side of the muscle.
The dotted
line across the tip of the paddle is usually ischemic and
can be proven so by the fluorescein and Wood's lamp test. Most
of this usually has to be sacrificed. |
|
|
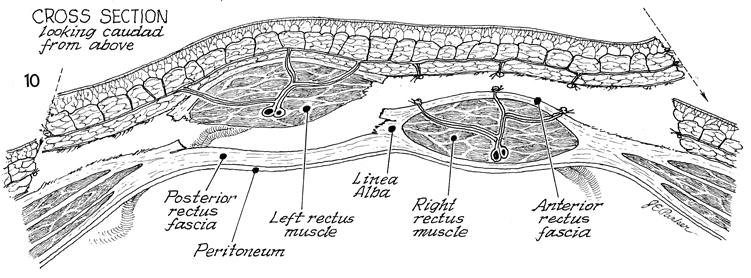
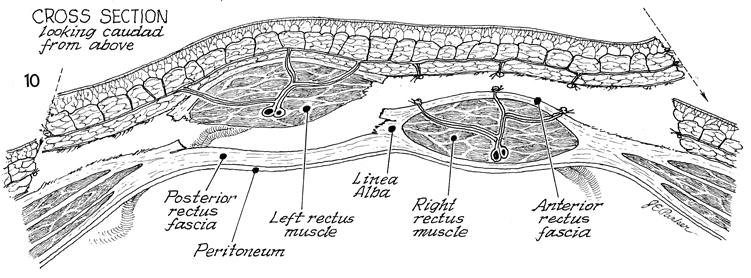
In
this cross section of the TRAM flap looking caudad from above,
the posterior rectus fascia is left intact. The inferior epigastric
vessels are shown entering the rectus muscle. The right rectus
muscle remains intact. The perforators coming off the anterior
rectus fascia have been ligated. The skin is cut at an angle.
The right side of this skin flap may have to be sacrificed
if it is shown to be ischemic under the Wood's lamp with fluorescein
dye injection. |
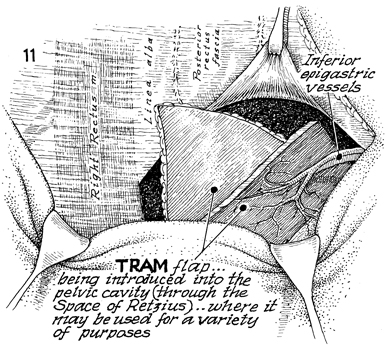
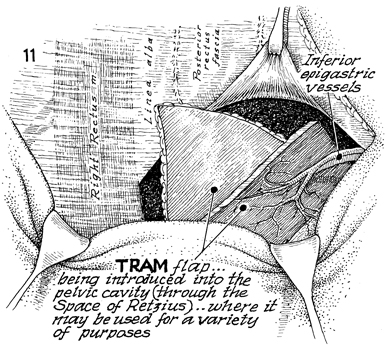
The TRAM flap is entering the abdominal cavity
through an incision in the posterior rectus fascia. It can be
brought down through the space of Retzius when the bladder has
been removed, or if the bladder is in place, it can be brought
down through the space of Retzius through the urogenital diaphragm
and into the vagina for a variety of purposes. |
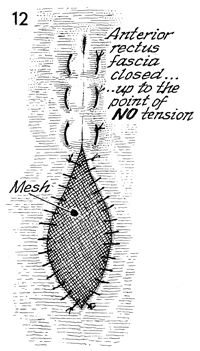
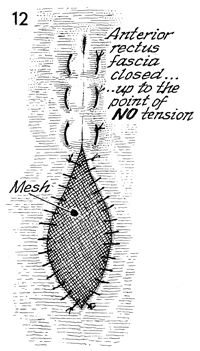
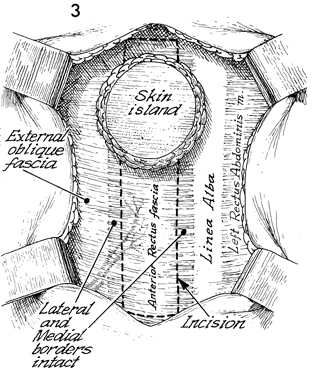
The anterior rectus fascia is closed up to
the point of no tension. At this point, a synthetic mesh can
be introduced into the defect and sutured into place. |
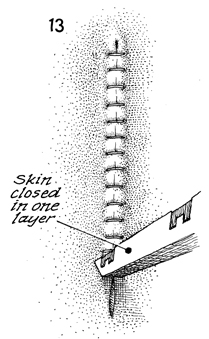
The skin is closed with stainless steel staples. |
|
|