Malignant
Disease:
Special Procedures
Staging
of Gynecologic
Oncology Patients With
Exploratory Laparotomy
Subclavian Port-A-Cath
Peritoneal Port-A-Cath
Application
of Vaginal
Cylinders for Intracavitary
Radiation Therapy
Application
of Uterine Afterloading Applicators
for Intracavitary Radiation Therapy
Pelvic High-Dose
Afterloader
Abdominal
Injection of Chromic Phosphate
( ) )
Supracolic
Total Omentectomy
Omental Pedicle "J"
Flap
Tube Gastrostomy
Total Vaginectomy
Radical
Vulvectomy
With Bilateral Inguinal
Lymph Node Dissection
Reconstruction
of the
Vulva With Gracilis Myocutaneous Flaps
Transverse
Rectus
Abdominis Myocutaneous
Flap and Vertical Rectus
Abdominis Myocutaneous
Flap
Radical
Wertheim
Hysterectomy With
Bilateral Pelvic Lymph
Node Dissection and With Extension of the Vagina
Anterior Exenteration
Posterior Exenteration
Total Pelvic
Exenteration
Colonic
"J" Pouch Rectal
Reservoir
Kock Pouch
Continent Urostomy
Omental "J" Flap
Neovagina
Ileocolic
Continent Urostomy (Miami Pouch)
Construction
of Neoanus
Gracilis Dynamic Anal
Myoplasty
Skin-Stretching
System Versus Skin Grafting
Gastric
Pelvic Flap for
Augmentation of Continent Urostomy or Neovagina
Control
of Hemorrhage in Gynecologic Surgery
Repair
of the Punctured
Vena Cava
Ligation
of a Lacerated
Internal Iliac Vein and
Suturing of a Lacerated Common Iliac Artery
Hemorrhage
Control in
Sacrospinous Ligament
Suspension of the Vagina
Presacral
Space
Hemorrhage Control
What
Not to Do in Case of Pelvic Hemorrhage
Packing
for Hemorrhage
Control
Control
of Hemorrhage
Associated With Abdominal Pregnancy |
Abdominal
Injection of
Chromic Phosphate ( ) )
 is indicated in those cases of ovarian carcinoma where all bulk
disease has been removed, and it is necessary to destroy tumor cells
or micronodules of tumor less than 4 mm in diameter. is indicated in those cases of ovarian carcinoma where all bulk
disease has been removed, and it is necessary to destroy tumor cells
or micronodules of tumor less than 4 mm in diameter.
Although a Silastic
catheter can be inserted at the time of laparotomy, it should not be
exteriorized but left in a subcutaneous pocket, because if it is exteriorized,
by the seventh or eighth postoperative day it will be grossly contaminated
and the patient will be at risk for peritonitis. Care should be taken
to ensure that there is no drainage of fluid from old closed suction
drain sites prior to injecting the radionucleotide.
The purpose of the
operation is to inject  into the peritoneal cavity in a manner that
will allow free flow of the fluid throughout the peritoneal cavity.
It should deliver 6000 rads to a depth of 3 mm on the peritoneal surfaces. into the peritoneal cavity in a manner that
will allow free flow of the fluid throughout the peritoneal cavity.
It should deliver 6000 rads to a depth of 3 mm on the peritoneal surfaces.
Physiologic Changes.  is an emitter of a beta
particle. The penetration power of a beta particle is 4 mm. It has
its effects on cells and micronodules of tumor. It is not effective
against bulk tumor. is an emitter of a beta
particle. The penetration power of a beta particle is 4 mm. It has
its effects on cells and micronodules of tumor. It is not effective
against bulk tumor.
Points of Caution. It is imperative that the paracentesis
needle be properly placed in the peritoneal cavity and not in an organ
or a pouch formed from postoperative adhesions.
Technique
|
|
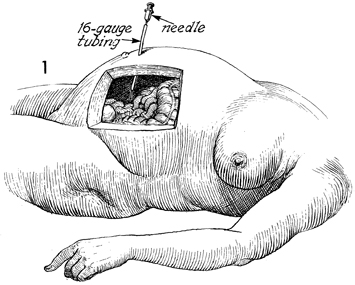
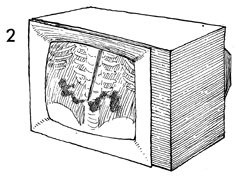
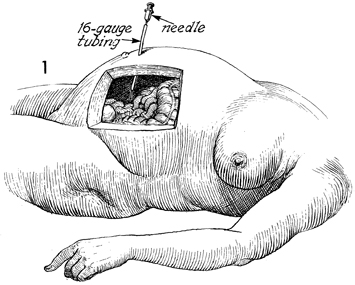
The
patient is placed in the supine position on the radiology fluoroscopy
table. A 16-gauge needle is used to perforate the anterior
abdominal wall under local anesthesia. A Silastic catheter
is threaded through the needle into the peritoneal cavity,
and a test dose of radiopaque dye and saline solution is injected
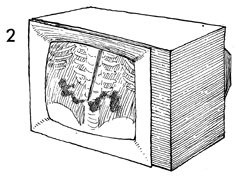
under fluoroscopic control. If the dye diffuses throughout
the abdomen and there is no pooling, the position of the catheter
is accepted. |
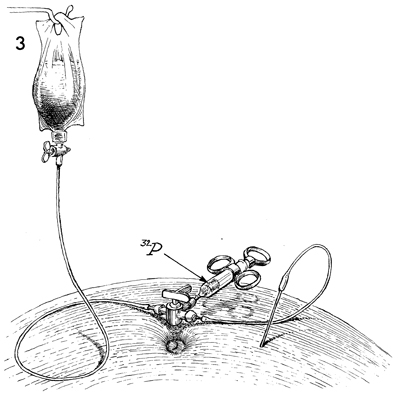
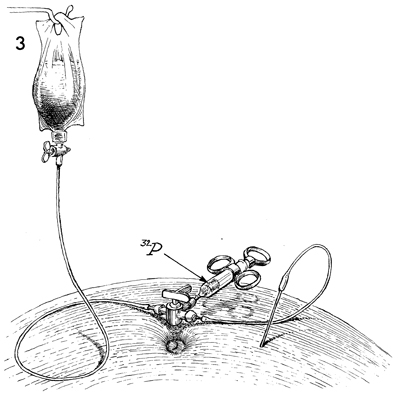
 is drawn up in a syringe, attached to
a three-way stopcock, and injected in one push. A container of
intravenous saline solution is then attached to the other arm
of the three-way stopcock, and 1000 mL are allowed to flow into
the peritoneal cavity, diluting the is drawn up in a syringe, attached to
a three-way stopcock, and injected in one push. A container of
intravenous saline solution is then attached to the other arm
of the three-way stopcock, and 1000 mL are allowed to flow into
the peritoneal cavity, diluting the  and promoting a flow
of the radionucleotide throughout the abdomen. and promoting a flow
of the radionucleotide throughout the abdomen. |
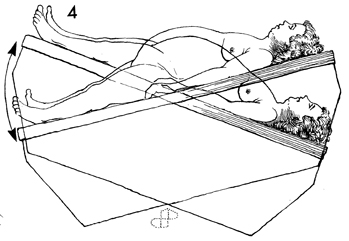
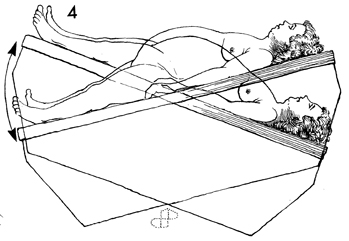
The patient is rotated from
side to side and from the Trendelenburg to reverse Trendelenburg
position to facilitate the spread of the radionucleotide over
the liver, under the diaphragm, and throughout the peritoneal
cavity. |
|