|
||||
Malignant
Disease: Staging
of Gynecologic Application
of Vaginal Application
of Uterine Afterloading Applicators Abdominal
Injection of Chromic Phosphate Radical
Vulvectomy Reconstruction
of the Transverse
Rectus Colonic
"J" Pouch Rectal Ileocolic Continent Urostomy (Miami Pouch) Construction
of Neoanus Skin-Stretching
System Versus Skin Grafting Gastric
Pelvic Flap for Control
of Hemorrhage in Gynecologic Surgery Repair
of the Punctured Ligation
of a Lacerated Hemorrhage
Control in Presacral
Space What
Not to Do in Case of Pelvic Hemorrhage Packing
for Hemorrhage Control
of Hemorrhage
|
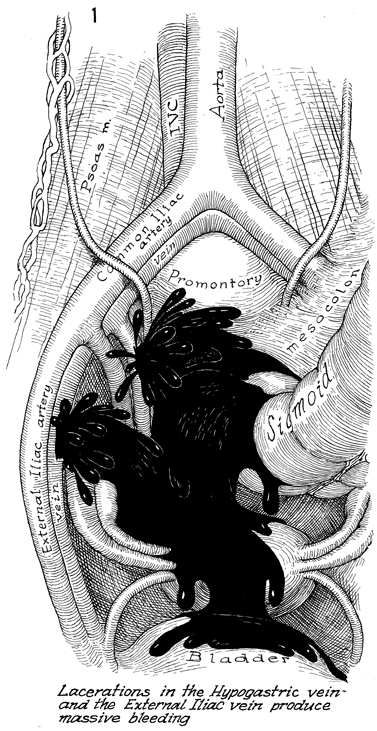
Packing for Hemorrhage Control Packing has made a popular return to trauma and pelvic surgery, based
on objective data. Every operative team should have its basic rules
concerning packing. Basically, when a hemorrhage has occurred and cannot
be controlled with the techniques mentioned in this section of the Atlas and
more than 10 units of blood have been administered, the patient will
start developing the signs and symptoms of hypovolemic shock. They
will be hypothermia and/or acidosis. The patient will also develop
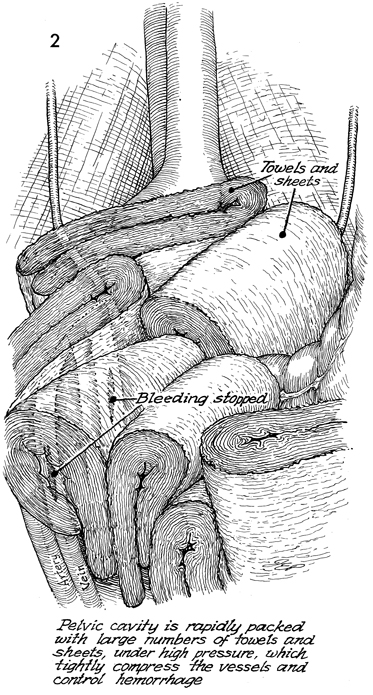
dilutional coagulopathy with bleeding from other sites. At this point, further attempts at vascular control are usually fruitless,
and it is efficacious to pack this area of the body with any large
sterile pack available. Extensive use of large packs is required; there
is no role for 4 X 4 sponges. Laparotomy packs may include tools, sheets,
and other aids to pack off this area in a proper manner. In closing the patient's abdomen the rectus fascia
should not be closed. The skin should be closed with towel clips. The
patient should be taken to the surgical intensive care unit. She should
remain intubated and on a mechanical respirator. Central venous access
must be made, and corrections must be started for all the signs and
symptoms of hypovolemic shock. The fascia should not be closed to prevent compartmental syndrome.
The large amount of packing necessary to control large vessels in the
pelvis can make ventilation extremely difficult, resulting in compartmental
syndrome. Forty-eight hours later, when all vital signs, electrolytes, hemoglobin,
prothrombin time (PT), and partial thromboplastin time (PTT) levels
have been corrected, the patient can be brought to the operating room,
the skin clamps and the packing can be carefully removed, and the surgeon
may frequently find little if any hemorrhage. If there is hemorrhage,
it can be properly controlled at this time with adequate operative
personnel and instruments. Technique
|
|||
Copyright - all rights reserved / Clifford R. Wheeless,
Jr., M.D. and Marcella L. Roenneburg, M.D.
All contents of this web site are copywrite protected.