|
||||
Malignant
Disease: Staging
of Gynecologic Application
of Vaginal Application
of Uterine Afterloading Applicators Abdominal
Injection of Chromic Phosphate Radical
Vulvectomy Reconstruction
of the Transverse
Rectus Colonic
"J" Pouch Rectal Ileocolic Continent Urostomy (Miami Pouch) Construction
of Neoanus Skin-Stretching
System Versus Skin Grafting Gastric
Pelvic Flap for Control
of Hemorrhage in Gynecologic Surgery Repair
of the Punctured Ligation
of a Lacerated Hemorrhage
Control in Presacral
Space What
Not to Do in Case of Pelvic Hemorrhage |
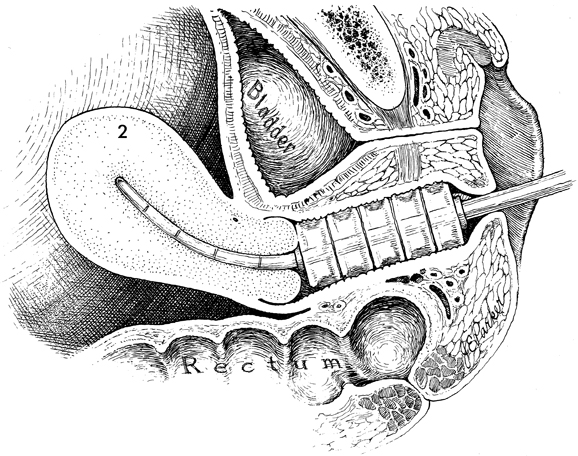
Application of Vaginal Cylinders for Vaginal intracavitary radiation therapy is applied for two reasons:
(1) to treat carcinoma directly in the vagina, the subvaginal mucosa
and, in adenocarcinoma of the endometrium, the lymphatic and (2) to
add radiation to point A in the isodose curve. The largest cylinder that can comfortably fit the vagina should be
used to achieve the most favorable isodose curve with the lowest surface
dose. An intrauterine tandem can be inserted through the vaginal cylinder
and can be loaded as the length of the uterus dictates. If the uterus
is absent, the cylinders can be used alone to apply radiation therapy
to the vagina. The purpose of applying intracavitary therapy to the vagina is to irradiate the vaginal canal with ionizing radiation. In general, attempts are made to deliver 4000 cGy of radiation to the depth dose of 1.5 cm. Physiologic Changes. The physiologic changes in this procedure are the same as for all procedures in which ionizing radiation is passed through normal and malignant tissue. Points of Caution. The vaginal cylinders should be
constructed so that they will fill the entire vaginal canal up to,
but not beyond, the introitus. Care should be taken that no radium
source extends beyond the vaginal introitus for fear that ulceration
of the labia minora and majora will occur. Fixation of the device should be made to ensure that the cylinder will not slip toward the introitus. This usually can be performed by suturing the labia together in the midline. Technique
|
|||
Copyright - all rights reserved / Clifford R. Wheeless,
Jr., M.D. and Marcella L. Roenneburg, M.D.
All contents of this web site are copywrite protected.